Introduction
Heart failure (HF) continues to be a major healthcare burden globally. The number of patients living with heart failure has increased over time for various reasons, including improved survival rates, a growing global population and recognition of entities such as heart failure with preserved ejection fraction, among others.1 Prevalence, however, varies greatly across the globe with Asia, specifically South-east Asia (SEA), recording some of the higher prevalence and mortality rates.2,3
Despite this, heart failure care remains unstructured within SEA. For example, in both Malaysia and Singapore, HF has yet to be recognised as a subspeciality and, although not specifically reported in the literature, this is fairly reflective of most other South-east Asian countries as well.4 Furthermore, formalised training in advanced HF and transplantation (AHFT) is mainly centred in Singapore.5 This is worrying, because the management of patients living with HF is often complex and recognition of clinically deteriorating patients living with HF often is beyond that of most core cardiology curricula. Furthermore, there is a widespread misconception that HF training and fellowship should be heavily focused on AHFT training (e.g. ventricular assist device implantation, heart transplantation) when, in fact, HF is multifaceted. In fact, ‘bread-and-butter’ HF practice normally revolves around optimisation of guideline-directed medical therapy, treatment of acute decompensation of HF, HF with preserved ejection fraction and cardiometabolic care, and occasionally patient selection for implantable device therapies (e.g. cardiac resynchronisation therapy or implantable cardiac defibrillators) or, more recently, transcatheter structural heart interventions.3,6,7
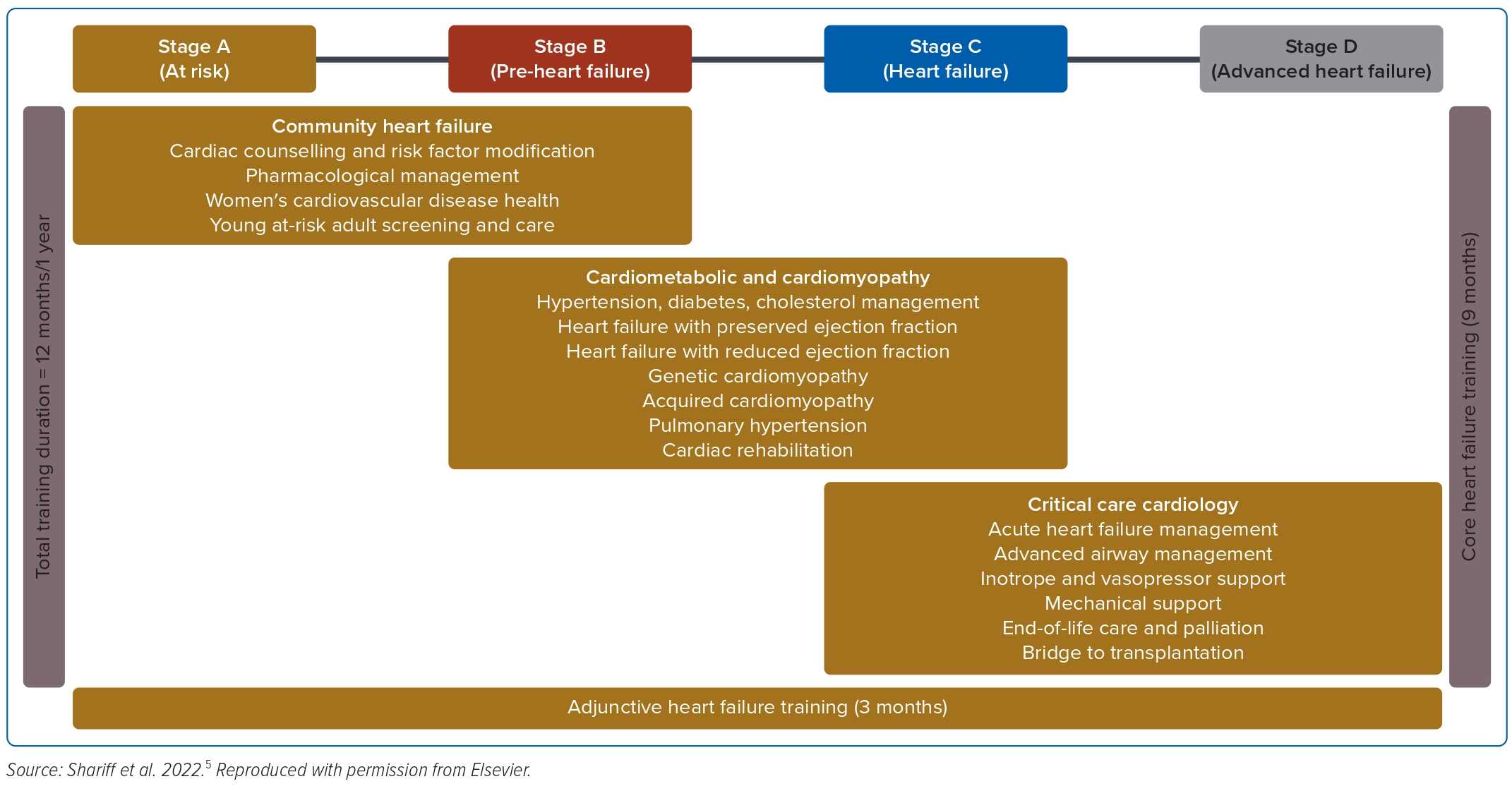
We recently made recommendations for a dedicated HF curriculum, built with SEA cardiologists and fellows-in-training (FIT) in mind (Figure 1).5 Following on from that publication, we felt that there was a great need to understand the thoughts and perceptions among cardiologists and FIT surrounding HF as a potential formalised subspeciality to be trained in. The aim of the present study was to gain an understanding of the knowledge, attitudes and perceptions of Malaysian cardiologists and FIT surrounding HF training and HF as a potential subspeciality.
Methods
We conducted a national-level survey study between 21 November and 20 December 2022 (1 month). The survey was designed using Google Forms and consisted of 28 items in total that surveyed the following areas of interest:
- respondent demographics;
- knowledge and perception of current clinical practice locally;
- knowledge, attitudes and perceptions of training in HF, associated cardiology subspecialities and AHFT; and
- attitudes and perceptions towards a recommended HF curriculum designed by the authors.
Some survey items provided multiple options, with respondents allowed to choose as many of the options provided they felt best answered the respective statement or question. Other survey items used a four-point Likert agreement scale to measure agreement with various statements or questions. Reporting guidelines were obtained through the EQUATOR network (https://www.equator-network.org). Respondents were invited to the take part in the survey through direct email communication using the database of existing cardiologists and FIT that is accessible via open access through both the National Heart Association of Malaysia and National Specialist Register database.8,9
Categorical variables are expressed as frequencies and percentages. Data analysis for free text items was performed using classic content analysis with inductive coding, with data review by two main investigators (RERS, SK).
The study was granted ethics approval by the Universiti Teknologi MARA (UiTM) Sungai Buloh Ethics Committee.
Results
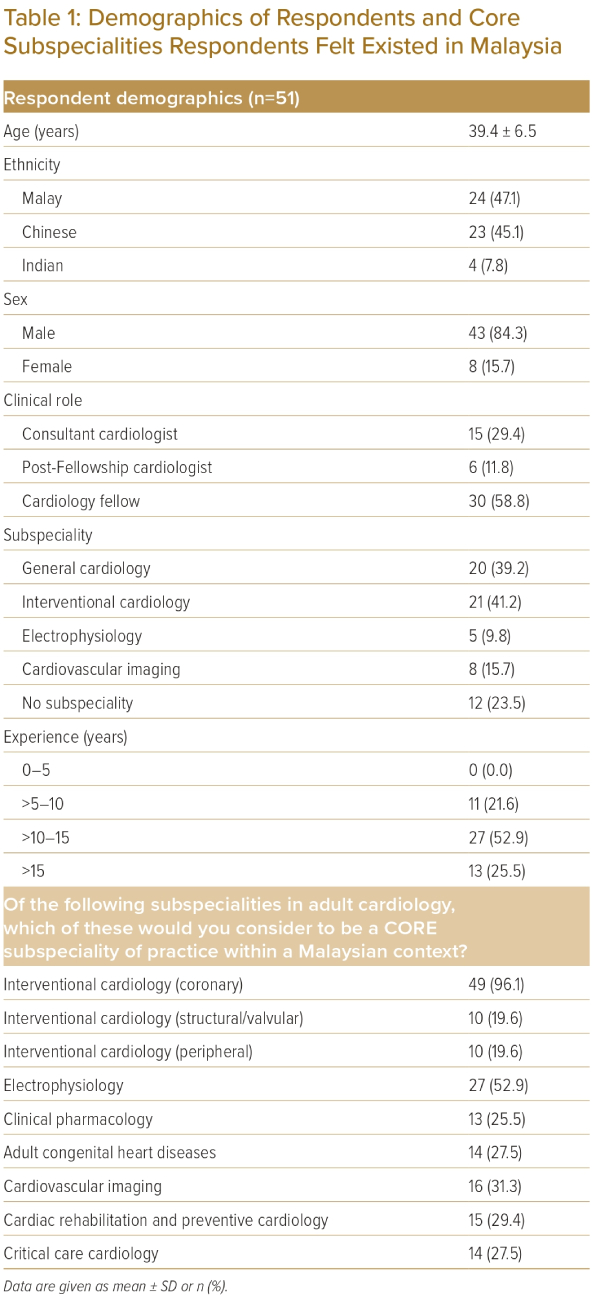
In all, 51 respondents (response rate 62.2%) completed the survey during the study period (Table 1). Of the 51 respondents, 43 (84.3%) were male. The mean (± SD) age of respondents was 39.4 ± 6.5 years. In terms of ethnicity, 47.1% of respondents were Malay, 45.1% were Chinese and 7.8% were Indian. Most respondents were FIT (58.8%), with the rest being post-Fellowship cardiologists (11.8%) and consultant cardiologists (29.4%). Most respondents self-identified as general cardiologists (39.2%) and interventional cardiologists (41.2%), and most had been practising for 10–15 years (52.9%) or for longer than 15 years (25.5%).
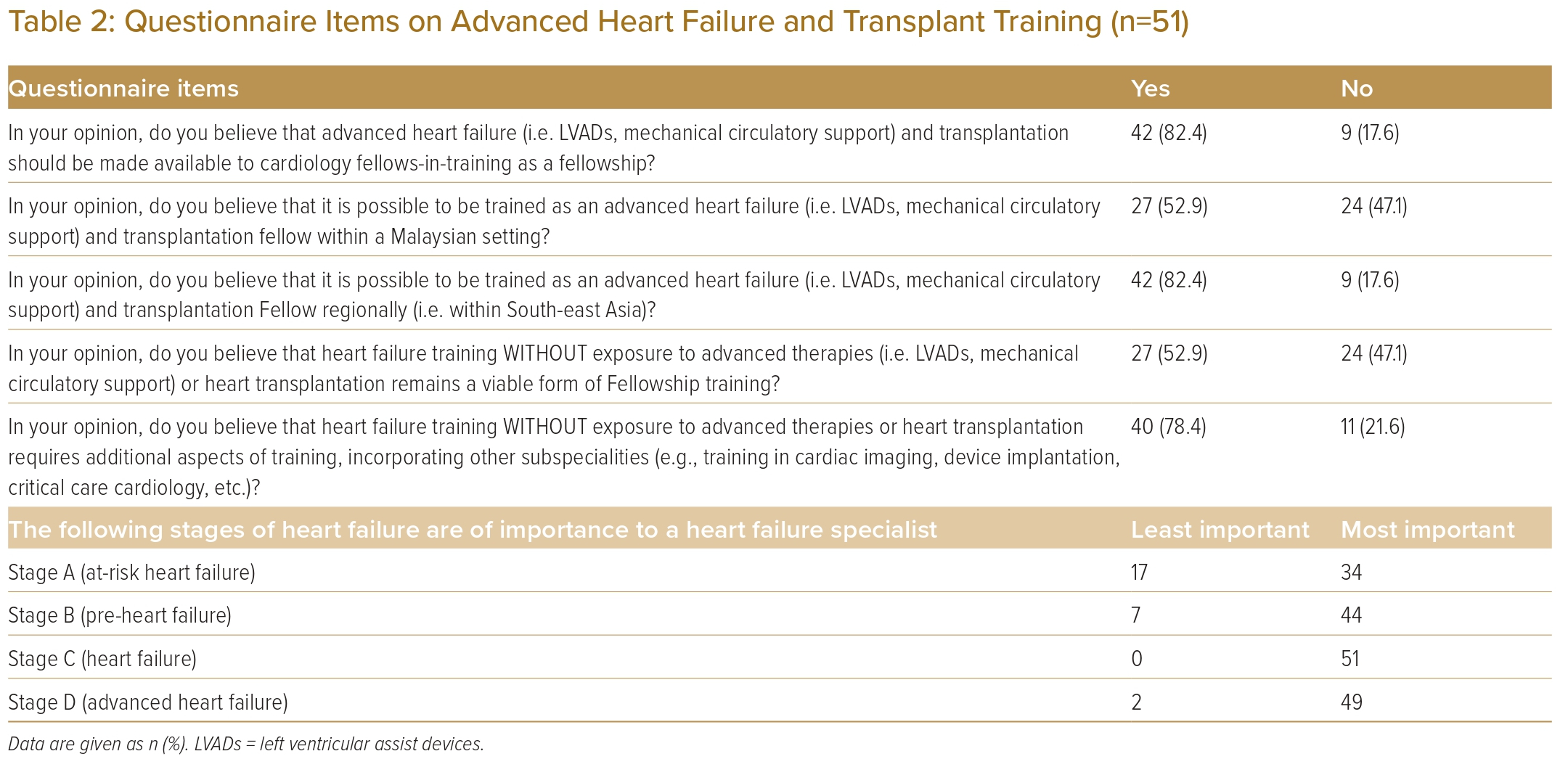
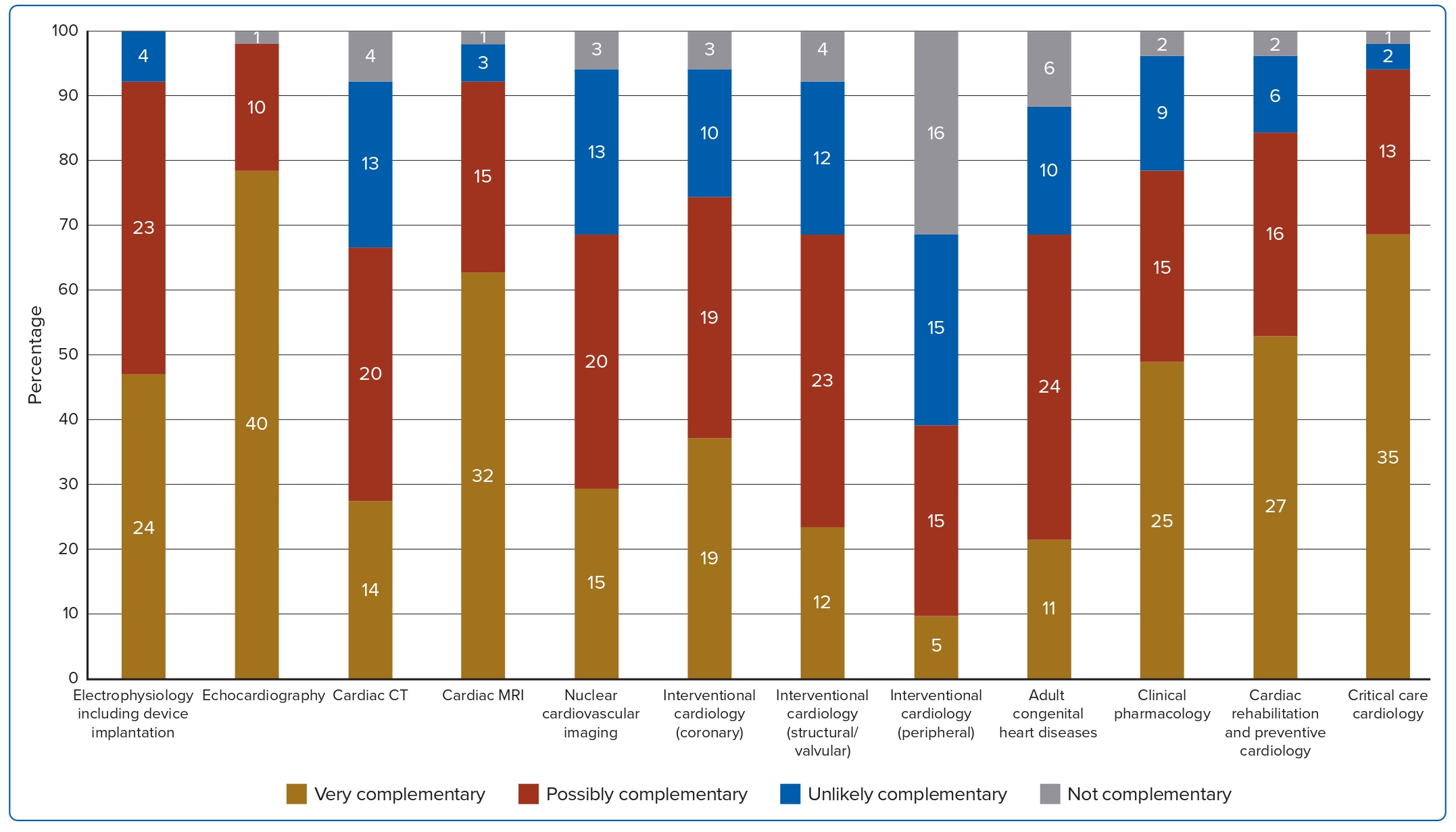
When asked about the current landscape in cardiology practice locally, most respondents felt that core subspecialities being practised in Malaysia include interventional cardiology (96.1%), cardiovascular imaging (31.3%) and electrophysiology (52.9%; Table 1). Although most felt that AHFT should be made available to FIT as an option for further Fellowship training (82.4%), there were far fewer who felt that this was feasible in our local setting (52.9%; Table 2). However, a considerable number (82.4%) felt that AHFT training is still feasible within the SEA region. Only 52.9% felt that HF training without exposure to AHFT would be worthwhile, and 78.4% felt that in the absence of AHFT training, adjunctive training in other cardiology subspecialities would be required. Most respondents felt that echocardiography (86.3%), cardiac MRI (52.9%) and critical care cardiology (68.6%) were possibly or very complementary training to HF (Supplementary Figure 1). When asked about potential barriers to establishing formalised HF training locally in Malaysia, most felt that the lack of heart transplantation and ventricular assist device implantation and financial constraints surrounding advanced therapies and transplantation were major concerns (Supplementary Figure 2). The perception that HF training is dependent on advanced therapies comes as no surprise, unfortunately. Despite recognising the role of the HF specialist in managing all stages of HF, most respondents felt that HF specialists have the most important role in managing patients primarily in stages C and D (Table 2).
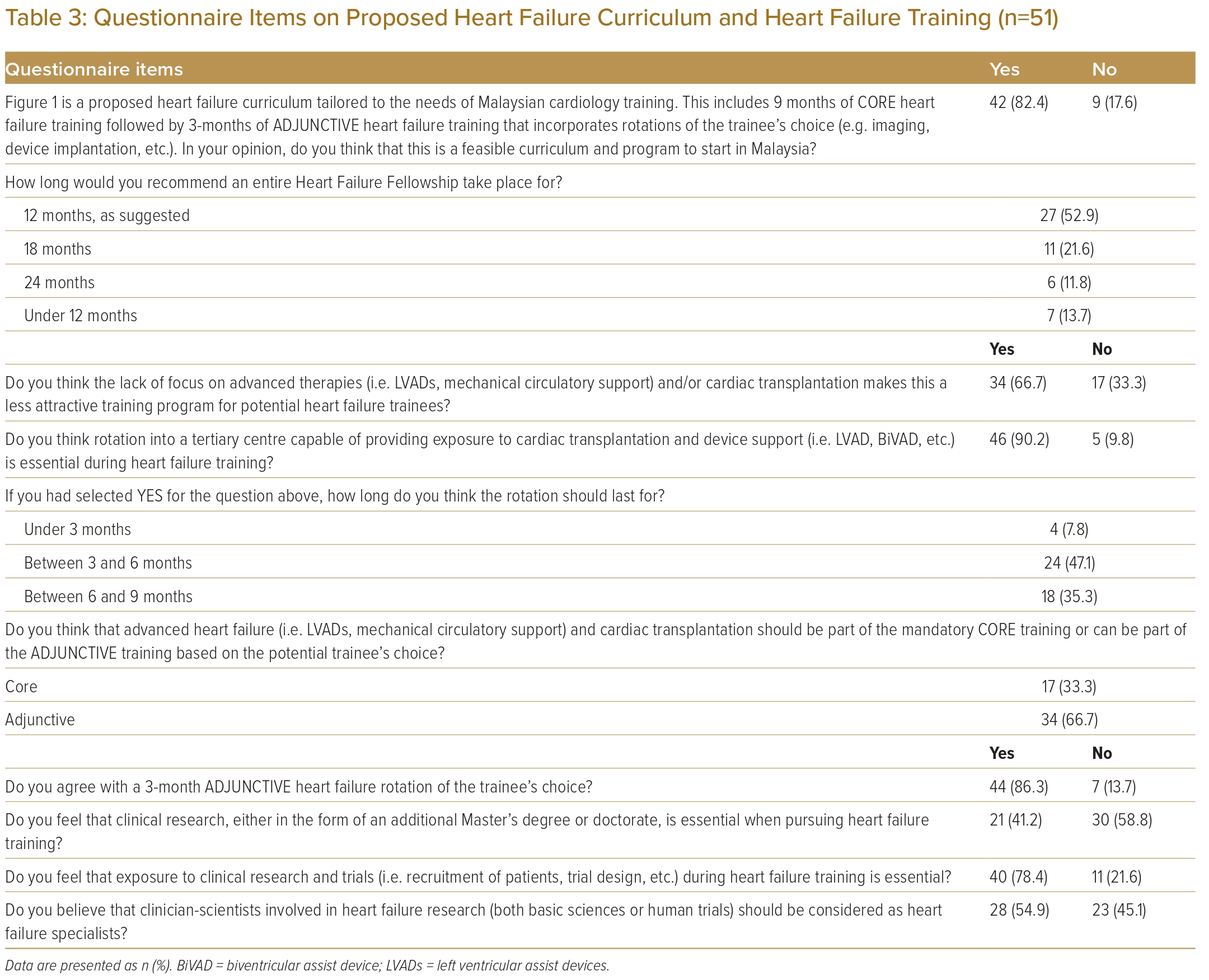
When introduced to our proposed curriculum (Fellowship) for HF training, 82.4% felt that it was reasonable (Table 3). Up to 33.4% of respondents felt that a longer training period was required, whereas 13.7% felt it should be shorter. Surprisingly, 66.7% felt that the lack of AHFT training made the Fellowship less appealing compared with a dedicated AHFT Fellowship, and most (90.2%) felt a rotation in a tertiary care centre with exposure to AHFT was essential during the training for at least 3–6 months (43.7%) or 6–9 months (35.3%). However, most (86.3%) agreed with an adjunctive 3-month elective period incorporating a subspeciality of the FIT’s choosing, with most, again, stating that echocardiography (78.4%), cardiac MRI (62.7%) and critical care cardiology (68.6%) were possibly or very complementary training to pursue (Figure 2). Although most respondents (78.4%) felt that exposure to clinical research and trials would be essential, a majority (58.8%) did not feel that formal training either in the form of a Master’s degree or doctorate was necessary while pursuing HF training. In fact, only 54.9% felt that clinician-scientists involved in HF research should be considered HF specialists.
Discussion
This survey provides novel insights into training in cardiology in Malaysia, and possibly in SEA as well. Training has always been structured around clinical fellowship, with a focus on obtaining practical cardiology skills, be it in the field of interventional cardiology, electrophysiology or cardiac imaging. A common opinion and possible reason why there remains a struggle in recognising HF as a formal subspeciality is that there is a lack of practical skills acquired during training. This is made worse by the lack of AHFT practice regionally, and low regard for research into and clinician-scientists in the field of HF.4
A potential solution to improve interest in HF fellowship training would be to incorporate other recognised popular subspecialities noted in our survey. This model of training is similar to that of the European Society of Cardiology’s HF training curriculum.10 The European curriculum recommends general HF training during the first year of fellowship, followed by an additional year of training in a field of the FIT’s choice, including cardiac imaging (specifically echocardiography, cardiac MRI or both), HF device implantation, AHFT or additional training in drugs, lifestyle and management. This is then supplemented by obtaining formal certification from the European Society of Cardiology’s Heart Failure Association. In fact, in the US, there has been a surge in recommendations surrounding incorporating critical care cardiology, aptly positioned as ‘critical care enrichment’, into advanced HF training.11–15 This may also be a way forward in developing a formalised HF training programme in SEA, focusing on haemodynamics, cardiogenic shock and mechanical circulatory support (areas of intersection between critical care medicine, interventional cardiology and acute HF management). Such recommendations have come to surface following criticism surrounding the current AHFT training model in the US as being ‘too narrow in its scope’ and ‘unfit for purpose’.16,17 Although the recommendations above would mean a longer duration of training in total, this seems to fit the current needs and wants of FITs, as suggested by the responses surrounding the expected duration of HF training in our survey.
Another area of concern, although ripe with opportunity, is the poor perception surrounding the benefit of formalised training in research and development within the field of HF. If anything, the exponential growth in drug and device development in the field of HF over the past two decades should be testament to how important research has been, and will continue to be, in this field.4 Careers built around conducting clinical trials and performing translational science should be encouraged because therapies such as heart transplantation may soon be made redundant by more novel and increasingly effective drug therapies. We have seen wonders with sacubitril–valsartan and sodium–glucose cotransporter-2 inhibitor trials in the past decade, so who is to say there will not be more advances beyond our present armamentarium?18
Conclusion
The mismatch between the training available and care provided for HF will continue to worsen over time as the burden of HF increases unless something is done to address it. This survey highlights several important issues surrounding knowledge and perception of current cardiology training in the SEA region, and how formal training in HF can be best implemented and potentially well received. As countries like the US have made major plans to overhaul the current AHFT system, in Malaysia we are in a position of privilege of only just starting out, allowing us to learn from others and tailor HF training to match our local needs. 
Click here to view Supplementary Material
Clinical Perspective
- Despite heart failure (HF) being a major contributor to the burden faced by regional healthcare services in South-east Asia, the degree of interest in the field among cardiologists remains unknown.
- At present, there are few structured programmes dedicated to formalised training in HF within South-east Asia.
- The main inertia in recognising HF as a subspeciality stems from a misconception that training requires exposure to advanced HF and transplantation , when in fact the field is multifaceted.