High-sensitivity cardiac troponin I (hs-TnI) is a specific biomarker for detecting myocardial injury.1 It plays a crucial role in diagnosing MI. Of note, hs-TnI can be detected in >50% of apparently healthy individuals.2
Silent ischaemia and non-ischaemic processes, such as cardiac abnormalities including left-ventricular hypertrophy, left-ventricular dysfunction, left-atrial enlargement, cardiac overload and inflammation, can lead to asymptomatic myocardial injury, which cardiac troponin I testing might detect.3–5 Accordingly, in individuals in whom cardiac troponin I is detected, there may be an association with cardiovascular (CV) risk factors. The role of assessing hs-TnI in terms of CV risk stratification is robust. However, there is growing evidence that an elevation in hs-TnI levels is significantly associated with adverse CV events.6–8 Furthermore, incorporating hs-TnI into the conventional risk factor model has the potential to enhance risk prediction.
Although most studies on the prognostic implications of hs-TnI have been conducted in Western populations with high CV risk, our objective is to investigate its prognostic significance specifically in a low-risk Asian population.6–10
Methods
Study Population
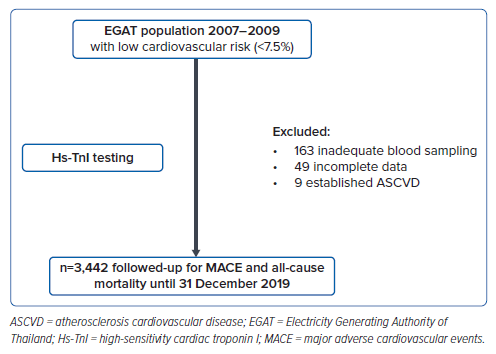
Data on individuals with low CV risk, as determined by having a Thai CV risk score <7.5% (Supplementary Table 1), were obtained from the EGAT study.11,12 This study was a longitudinal prospective cohort study conducted during the 2007–2009 survey period (cohorts 1–3). Participants who had been diagnosed with atherosclerotic CV disease prior to enrolment were excluded from the study.
All participants underwent a comprehensive assessment, including demographic data collection, physical examinations conducted by a trained physician and blood testing. The blood tests included total cholesterol, HDL, LDL, triglyceride levels, creatinine and other blood chemistry parameters.
High-sensitivity Cardiac Troponin I
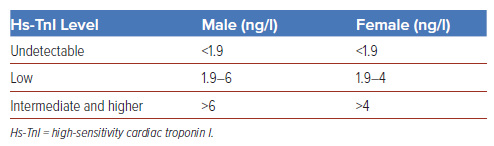
Blood samples from participants, which had been stored at minus 80°C, were thawed then centrifuged prior to testing. For the hs-TnI testing process, an ARCHITECT STAT assay (Abbott Laboratories) was used. This assay has a detectability range of 1.9–50,000 ng/l and incorporates sex-specific cut points.13 Based on the results of the low CV risk population, participants were categorised into three different groups: undetectable hs-TnI, low hs-TnI and intermediate and higher hs-TnI (Table 1).
Outcomes
Participants were followed-up for the occurrence of major adverse cardiovascular events (MACE), defined as death from CV causes, nonfatal MI and nonfatal stroke, until 31 December 2019. The incidence of all-cause mortality was also monitored during this period. The study flow is depicted in Figure 1. Information regarding CV events was obtained by cross-referencing participants’ Thai National Identification numbers with the national health reimbursement database system using ICD-10 codes (acute MI: I21; unstable angina: I20.0; stroke: I63). This information was then rechecked by telephone calls or home visits, along with a request for documentation from hospitals to verify the diagnosis and confirm vital status. The diagnosis and vital status confirmation were reviewed by specialists, including neurologists and cardiologists.
Statistical Analysis
Hs-TnI is reported as median and interquartile range. Other baseline characteristics, including age, sex, weight, height, waist circumference, systolic blood pressure (SBP), comorbidities and laboratory results, are presented as mean and SD for continuous variables and frequency and percentage (%) for categorical variables. Fisher’s exact test or χ2 test were used to determine differences between groups and independent Student’s t-test was used for continuous data. Univariate and multivariate analyses were used to analyse factors associated with MACE. Hs-TnI was classified into undetectable hs-TnI, low hs-TnI and intermediate and higher hs-TnI. Kaplan–Meier curve analysis and Cox proportional hazard models were used to determine the association of hs-TnI level and MACE compared with intermediate and higher hs-TnI for the primary outcome and other end points including all-cause mortality, CV death, MI (fatal MI, nonfatal MI), cerebrovascular events (fatal and nonfatal stroke) and a composite of MACE and all-cause death. Conventional risk factors (age, sex, SBP, diabetes, smoking status and estimated glomerular filtration rate) were adjustment factors in the model. Furthermore, subgroup analyses were also performed in populations defined by Thai CV risk score (<5% or 5–7.5%), sex, hypertension (yes/no), diabetes (yes/no), smoking status and BMI (<27, ≥27 kg/m2). p<0.05 was considered significant. All analyses were performed using SPSS V.22.0 (IBM).
Results
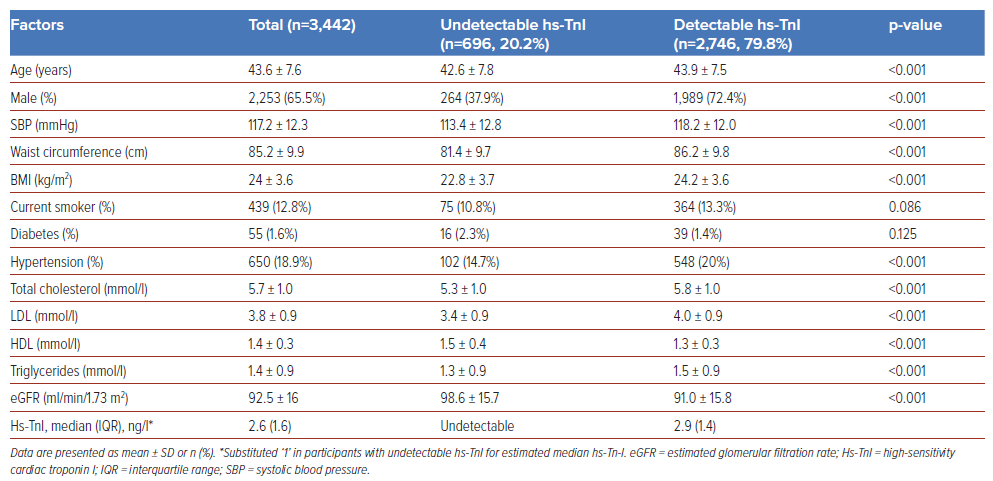
Of the 3,663 EGAT participants with low CV risk (<7.5%), 3,442 individuals who completed data and blood sampling were enrolled in this study. The mean age of the participants was 43.6 years; 65.5% were male. Hs-TnI was detected in 79.8% of the participants; the median hs-TnI level was 2.6 ng/l (IQR 1.6). Baseline characteristics between the undetectable hs-TnI and detectable hs-TnI groups are presented in Table 2. During a median follow-up period of 10.3 years, 52 events (1.5%) of MACE and 60 events (1.7%) of all-cause mortality occurred. Causes of death are presented in Supplementary Table 2. The univariate analysis revealed that hs-TnI, age, male sex, systolic blood pressure (SBP), waist circumference, BMI and triglyceride levels were significantly associated with the incidence of MACE; after adjusting for conventional risk factors, an increasing level of hs-TnI remained significantly associated with the incidence of MACE (HR 1.03; 95% CI [1.02–1.04] p<0.001; Supplementary Table 3). The area under the receiver operating characteristic curve (AUC) for hs-TnI to predict major CV events was 0.658 (95% CI [0.588–0.729]; p<0.001). The cut-off value of hs-TnI for major CV events was 2.85 ng/l. This cut-off value had 65.4% sensitivity and 58.5% specificity. In men, the cut-off value of hs-TnI was also 2.85 ng/l, with a sensitivity of 65.9% and specificity of 48.2% (AUC 0.599; 95% CI [0.513–0.684]; p=0.025). In women, the cut-off value was 2.55 ng/l with 87.5% sensitivity and 68.9% specificity (AUC 0.756; 95% CI [0.588–0.924]; p=0.012; Supplementary Figures 1–3).
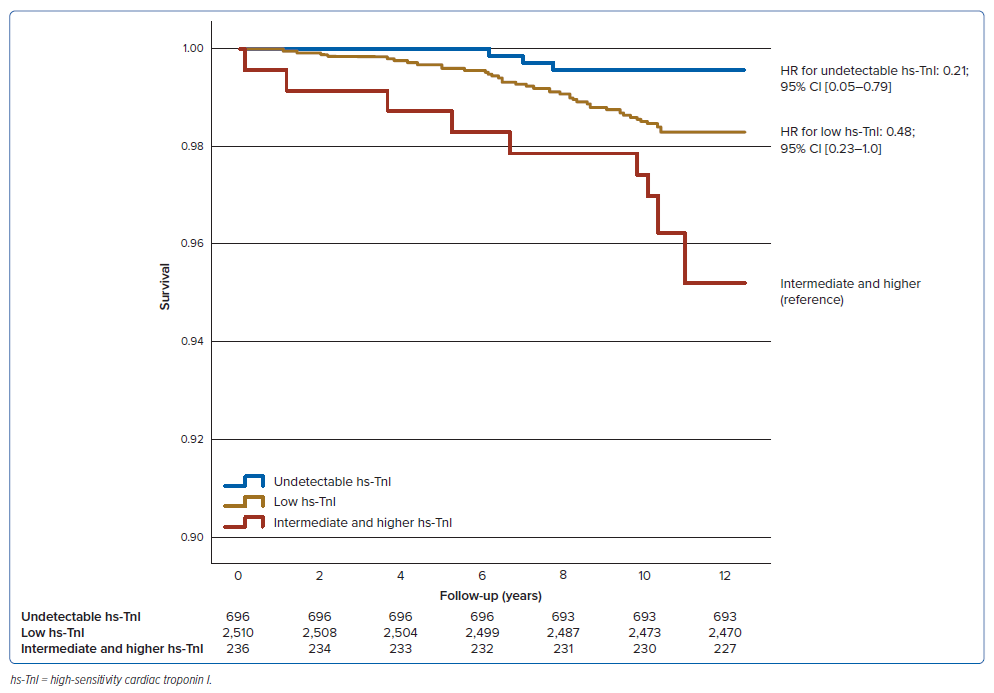
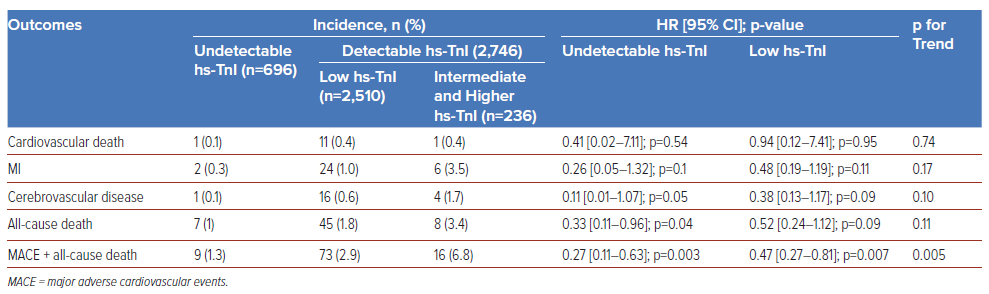
Compared with the intermediate and higher hs-TnI group, the undetectable hs-TnI group and the low hs-TnI group had 79% and 52% lower incidences of MACE, respectively (HR 0.21; 95% CI [0.05–0.79] and 0.48; 95% CI [0.23–1.0]; p for trend 0.045; Figure 2). Similarly, the undetectable hs-TnI and low hs-TnI group also had significantly lower rates of composite MACE and all-cause mortality compared with the intermediate and higher hs-TnI groups (HR 0.27; 95% CI [0.11–0.63] and 0.47; 95% CI [0.27–0.81]; p for trend 0.005; Table 3). Additionally, other endpoints including CV death, MI and cerebrovascular events also showed a trend of lower incidence in the undetectable hs-TnI group, but the differences were not statistically significant (Table 3). Subgroup analysis indicated that the incidence of MACE remained higher in individuals with either extremely low or low CV risk compared with those with undetectable hs-TnI (p for interaction 0.83). No significant differences were observed between other subgroups (Supplementary Figure 4).
For low-CV-risk individuals (5–7.5%) with detectable hs-TnI, the rate of MACE was nearly three events per 1,000 person-years, whereas in cases where hs-TnI was undetectable, the event rate was one per 1,000 person-years. Extremely low-CV-risk individuals (<5%) with undetectable hs-TnI also demonstrated lower event rates compared with those with detectable hs-TnI (0.32 versus 1.23 events per 1,000 person-years). Similarly, MI occurred at a lower rate in individuals with undetectable hs-TnI, both in the extremely low- and low-CV-risk groups. (Supplementary Figure 5)
Our study also revealed that being female, younger (<35 years old), non-obese (BMI <27 kg/m2, waist circumference <80 cm), lower LDL (<3.4 mmol/l), higher HDL (≥1 mmol/l), lower triglycerides (<1.7 mmol/l), SBP <120 mmHg and diastolic blood pressure (DBP) <90 mmHg were significantly associated with undetectable hs-TnI (Supplementary Table 4).
Discussion
The study has three main findings. First, in a low-CV-risk Thai population (risk score <7.5%), 79.8% of participants had detectable hs-TnI. Second, having a higher level of hs-TnI was significantly associated with the incidence of MACE. Conversely, participants with undetectable hs-TnI had a significantly lower incidence of MACE and all-cause mortality compared with the intermediate and higher hs-TnI group. Third, subgroup analysis revealed that the incidence of MACE remained higher in participants with detected hs-TnI, even in the extremely low- or low-CV-risk categories, compared with those with undetectable hs-TnI.
This study demonstrates that low levels of detectable hs-TnI in the Thai low-CV-risk population are significantly associated with an increased incidence of MACE. This observation is consistent with several studies conducted in Western countries, where hs-TnI in asymptomatic individuals has provided significant long-term prognostication for CV risk.6–10 The detectable rate of hs-TnI in our present study aligns with that of other studies, such as MORGAM, ARIC and the Gutenberg Health Study, which reported detectable rates ranging from 74.8% to 85%.6,14,15 In contrast, the JUPITER study exhibited a significantly higher detected hs-TnI rate of almost 92%, potentially explained by the elevated high-sensitivity C-reactive protein levels in the JUPITER population, indicative of a non-low-risk population.16
The median hs-TnI in the current study was slightly lower than that in the study by Abe et al. of 698 apparently healthy Japanese subjects (2.6 ng/l versus 3.2 ng/l, respectively), which may be because of a more elderly population in the study by Abe et al.17 The authors also found that troponin I level showed significant associations with male sex and BMI, which correlates with our findings. The detectable hs-TnI group had a higher proportion of males, individuals with a higher BMI, current smokers, hypertension and high LDL, all of which are well-known CV risk factors, compared with the undetectable hs-TnI group.
The prevalence of diabetes was slightly higher in the undetectable hs-TnI group than in the detectable hs-TnI group, although this difference was not statistically significant. While current smoking was inversely associated with MACE, the relationship was nonsignificant. Therefore, the effects of smoking may be related to intensification factors such as the intensity of smoking, duration and time since cessation. Smoking status alone was insufficient to precisely demonstrate the effects of smoking. Thiravetyan and Vathesatogkit revealed a significant increase in risks for all-cause mortality, CV mortality and MACE among current and ex-smokers compared with never smokers, based on a 30-year EGAT cohort study.18
Our findings also demonstrate an association between hs-TnI level and the incidence of MACE. Specifically, individuals with intermediate and higher hs-TnI levels (hs-TnI >6 ng/l in males, hs-TnI >4 ng/l in females) and low hs-TnI levels (hs-TnI 1.9–6 ng/l in males, hs-TnI 1.9–4 in females) were at an approximately five-fold and two-fold increased risk of MACE, respectively, irrespective of traditional CV risk factors, compared with those with undetectable hs-TnI. This observation is similar to the results from the BiomarCaRE study, which indicated a stepwise elevation in the risk of a first CV event with increasing hs-TnI quintiles (2.5, 2.8, 5.4 and 5.9 ng/l).7 The rate of MACE and MI was notably lower in the group with undetectable hs-TnI compared with the group with detectable hs-TnI, even when considering low-risk populations categorised into extremely low and low risk (0–5% and 5–7.5%).
Hs-TnI is a biomarker primarily associated with cardiac muscle damage. In the general population, the mechanisms underlying the relationship between hs-TnI and adverse CV outcomes can be complex and multifactorial. This relationship includes subclinical damage to cardiomyocytes because of factors such as endothelial and microvascular dysfunction, inflammation, oxidative stress and elevated blood pressure.19 Metabolic abnormalities, such as diabetes, dyslipidaemia and obesity, can impact the heart and blood vessels, increasing the risk of cardiac damage and subsequent hs-TnI release.20 Other conditions such as AF may also lead to modest troponin release.21 Hs-TnI can also be influenced by various CV risk factors, such as age, sex, smoking and family history. Consequently, these factors can contribute to the likelihood of cardiac damage and atherosclerosis, potentially leading to hs-TnI elevation.22 A recent study demonstrated correlations between the severity of coronary atherosclerosis and cardiac troponin concentration determined by coronary angiography. This finding also supports the notion that ‘troponin leakage’ may result from subclinical coronary atherosclerosis.23
Moreover, hs-TnI assays are designed to detect extremely low levels of troponin I in the blood, enabling the identification of even small amounts of cardiac muscle damage. The elevation of hs-TnI might indicate subclinical atherosclerosis, which increases CV risk, and can enhance risk stratification to identify those at higher risk who could benefit from timely preventive interventions to reduce the risk of adverse CV events. This is supported by the results of the WOSCOPS trial, which demonstrated that hs-TnI concentration significantly predicted coronary events. Pravastatin significantly lowered hs-TnI by 13% (10–15%; placebo-adjusted, p<0.001) at 1-year follow-up and reduced CV disease at 5 and 15 years follow-up, independent of cholesterol lowering.24
According to the 2019 American College of Cardiology/American Heart Association guideline on the primary prevention of CV disease, it is recommended to consider risk-enhancing factors in individuals with borderline risk (5–7.5% 10-year atherosclerosis cardiovascular disease [ASCVD] risk) and intermediate risk (7.5–20% 10-year ASCVD risk).25 These factors include having a family history of premature ASCVD, chronic inflammatory disease, South Asian ancestry, a history of preeclampsia or preterm delivery, early menopause, erectile dysfunction, chronic kidney disease, metabolic syndrome, persistently elevated inflammatory markers or elevated lipid biomarkers.25 Therefore, the elevation of hs-TnI among individuals with borderline risk (5–7.5%) may serve as a risk-enhancing factor, indicating that moderate-intensity statin therapy may be considered. However, this approach should be formally addressed in well-designed prospective studies in the future. While hs-TnI concentrations <5 ng/l identify patients who present with clinically suspected acute coronary syndrome at the emergency department as low risk, this group has a 1-year incidence of MI and CV death of 0.6%26. Therefore, the rule-out algorithm recommends discharging low-risk patients from the emergency department and possible follow-up as outpatients.27 Subsequently, we should promptly assess CV risk and consider primary intervention if indicated in those with detectable hs-TnI (>1.9 ng/l).
In cases where the risk decision is uncertain in terms of primary prevention, the use of coronary calcium score may be considered for risk discussion and guiding further preventive management. Similarly, individuals with undetectable hs-TnI exhibit very low CV risk. Therefore, we propose that undetectable hs-TnI may also serve as a de-risking marker for individuals with uncertain risk profiles. Using hs-TnI testing, which is simpler, widely accessible, and devoid of radiation exposure compared with coronary artery calcium testing, could substantially facilitate the identification of individuals at very low risk for future CV events. Finally, further research on cardiac troponin across various clinical settings, particularly regarding its role in assessing CV risk, is warranted.
There are some limitations to our study. First, the participants in this study were employees of a state-owned electricity enterprise under the supervision of the Ministry of Energy of Thailand, mostly based in urban areas, which might not fully represent the majority population of Thailand. Second, we did not assess the impact of medications on the participants; certain medications could potentially reduce CV risk.
Our study has several strengths. First, this is the first study in Asia demonstrating the ability of hs-TnI testing to provide risk prognostication for individuals with low CV risk. Second, this study followed participants for a decade (median time follow-up 10.3 years) in a well-established longitudinal cohort study in Thailand with validated outcomes. Lastly, our study suggests that undetectable hs-TnI could serve as a negative risk marker. Further studies should be conducted to evaluate the role of hs-TnI in terms of de-risking marker.
Conclusion
In conclusion, hs-TnI testing can provide risk prognostication among Thai individuals with low CV risk. Hs-TnI is significantly associated with the incidence of MACE and conversely, undetectable hs-TnI also serves as a negative risk marker for MACE.
Clinical Perspective
- High-sensitivity cardiac troponin I (hs-TnI) provides risk prognostication in the general population.
- The absence of detectable hs-TnI could serve as a negative risk marker for major adverse cardiac events.
- Similar to having a coronary artery calcium score of zero, undetectable hs-TnI might play a role as a de-risking marker.