The World Health Organization’s Global Health Observatory 2019 reports that people worldwide are living longer. By 2050, the world’s population aged ≥60 years is expected to reach 2 billion, up from 900 million in 2015.1 The shift in the distribution of the population towards older age started in high-income countries, with the proportion of the population aged ≥60 years in Japan reaching >30% in 2017.1 The most significant changes in population age structure are currently being experienced in lower- and middle-income countries.1 The Global Health Observatory’s 2019 report lists ischaemic heart disease and stroke as the top two causes of death globally, accounting for 16% and 11% of total deaths worldwide, respectively.1 These two conditions have been the top two causes of death globally since 2000. Even in low-income countries, ischaemic heart disease is the third leading cause of death after neonatal and infectious causes. However, there is little evidence suggesting that older people generally are in better health. Globally, the main contributor to disability-adjusted life years (DALY), after neonatal conditions, is the ischaemic heart disease burden.1
The MSD Manual ( https://www.msdmanuals.com/professional; accessed 23 October 2021) defines elderly or geriatric as age >65 years, but most people do not require expert geriatric care at 70, 75, or even 80 years of age. Most cardiac intervention trials do not include elderly patients, with studies in the elderly primarily from subgroup analyses of major trials. In the setting of acute coronary syndrome (ACS), subgroup analysis from many randomised control trials, such as PAMI-1, GUSTO-IIb, and DANAMI-2, has shown significant reductions in the combined endpoint of death, stroke and reinfarction in the percutaneous coronary intervention (PCI) arm compared with fibrinolysis in elderly patients with ST-elevation MI (STEMI). A meta-analysis of the SENIOR PAMI, TACTICS TIMI-RCT and PCAT-2 trials also found favourable outcomes in the elderly group undergoing cardiac intervention compared with medical therapy.2 In all these trials, patients in the very elderly group (age >80 years) are underrepresented. As such, clinicians are less assertive when it comes to providing cardiac intervention in elderly patients.
Long-term mortality is similar in elderly patients (age >80 years) treated with coronary artery bypass graft (CABG) surgery or PCI, but reintervention is higher in the coronary intervention group.3,4 Conrotto et al. reported that the risk for the primary composite endpoint of all-cause death, cerebrovascular accident and MI in very elderly patients was similar between those undergoing PCI versus CABG, despite a greater prevalence of baseline comorbidities in the PCI group.4 Another meta-analysis of 32 studies of PCI performed in patients aged ≥80 years found a pooled 30-day estimate of mortality of 5.4% and a 1-year survival estimate of 87%.5
The aim of this study was to investigate the safety outcomes by analysing total all-cause mortality and major adverse cardiovascular events (MACE) during the periprocedural period (up to 30 days) and 1 year after PCI in a cohort of the elderly patients stratified according to age (70–74, 75–79 and ≥80 years old). In addition, we analysed the relationships between these cardiovascular outcomes and both clinical characteristics and elective/urgent PCI status. Overall survival curves across all age groups were also analysed.
Methods
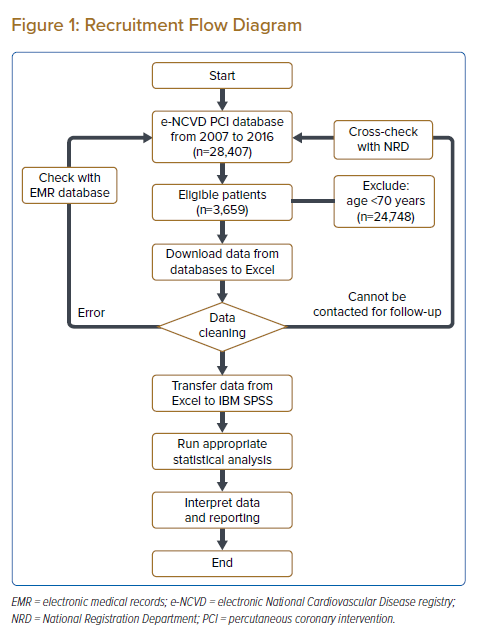
This study was a single-centre retrospective cross-sectional study that included every elderly patient (age ≥70 years) who underwent PCI between 2007 and 2016. Data were collected through an electronic medical record (EMR) database at Institute Jantung Negara (National Heart Institute), Kuala Lumpur, Malaysia (the national cardiovascular referral centre). The study was approved by the Institutional Research Ethics Committee of the Institute Jantung Negara.
Patients admitted to the Institute Jantung Negara between 2007 and 2016 who underwent PCI as either an urgent or elective procedure were screened for inclusion in this study. Within this population, all patients who were aged ≥70 years at the time of admission were in the study. Patients <70 years of age were excluded from the study. Urgent PCI was defined as an admission for ACS with the patient requiring PCI immediately upon admission; STEMI, both primary and rescue, ongoing chest pain with unstable angina (UA) or non-STEMI (NSTEMI). Elective PCI was defined as a planned admission for PCI because of symptoms, positive results on functional studies, staged PCI/post ACS; facilitated/pharmaco-invasive/delayed PCI among stable ACS patients or referral from other centres. Most of the patients included in the study were Malaysian (Malay, Chinese, Indians and other indigenous people of Malaysia, such as Orang Asli, Iban and Kadazan, among others).
Baseline patient characteristics, including demographics (sex, age, PCI status [elective or urgent]) and comorbidities (smoking, dyslipidaemia, hypertension, diabetes, history of ischaemic heart disease, family history of ischaemic heart disease, heart failure, defined as heart failure with a significantly reduced left ventricular ejection fraction [LVEF] ≤35%, cerebrovascular accident, chronic renal failure), were compared between the three predetermined age groups: early-elderly (age 70–74 years), mid-elderly (age 75–79 years) and late-elderly (age ≥80 years).
All hospital admissions, readmissions and redo PCI data were collected from electronic medical records. MACE was defined as a composite of total cardiovascular events, including fatal and non-fatal MI/stroke, hospitalisation for revascularisation, stent thrombosis and angiographic target vessel revascularisation (TVR)/target lesion revascularisation (TLR). TVR was defined as any repeat intervention to any segment of the previously intervened vessel, including upstream and downstream branches. TLR was defined as an intervention to a segment of a previously intervened target vessel. In all, 42 angiograms were reviewed to determine TVR/TLR. Information regarding clinical status was collected based on follow-up obtained 1 year after the procedure during a clinic visits, via telephone interviews or from the Malaysia National Cardiovascular Disease Registry database and cross-checked against the Malaysia National Registration Department if the patient could not be contacted or had died.
The revascularisation strategy was determined by the treating interventional cardiologist in the institution and included plain old balloon angioplasty (POBA), implantation of a drug-eluting balloon or drug-eluting stent, atherectomy on any native vessels and grafts; all strategies were accepted and included in the study. In addition, therapy with any single antiplatelet agent (due to bleeding risk) or dual antiplatelet therapy (e.g. aspirin or triflusal with clopidogrel, prasugrel, ticlopidine or cilostazol) was also accepted.
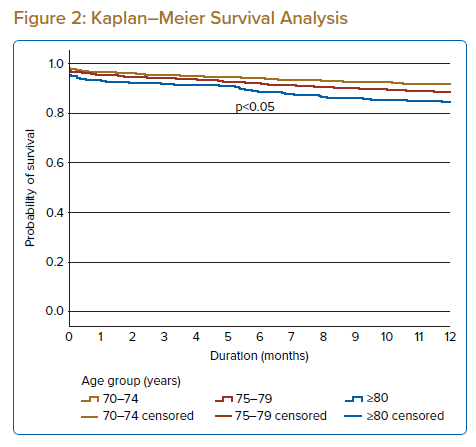
All statistics are descriptive. Data are presented as percentages or the mean ± SD. The significance of differences in proportions was tested with the Chi-squared test. Logistic regression was used to describe relationships. Cumulative events curves were generated using the Kaplan–Meier method.
Results
Over the 10 years from 2007 to 2016, 28,407 patients were admitted to the Cardiology Department at Institute Jantung Negara and underwent PCI (either urgent or elective). Of these patients, 3,659 (12.9%) were aged ≥70 years at the time of admission. After further evaluation, all these patients were found to be eligible for inclusion in this study (Figure 1). Of the 3,659 patients included in the study, 3,175 (86.8%) completed at least 1 year of follow-up (via clinic visits, telephone interviews or inclusion in the National Cardiovascular Disease Registry database); data for 463 (12.7%) patients were obtained through cross-checks with the National Registration Department. The 21 (0.6%) patients who were lost to follow-up were also included in the study. Most of the patients lost to follow-up were from other states in Malaysia, with logistical or financial constraints being the leading causes of loss to follow-up.
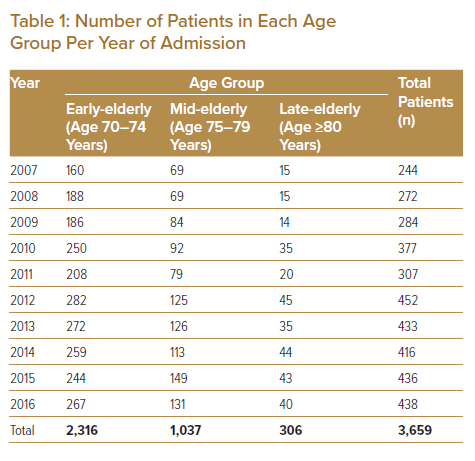
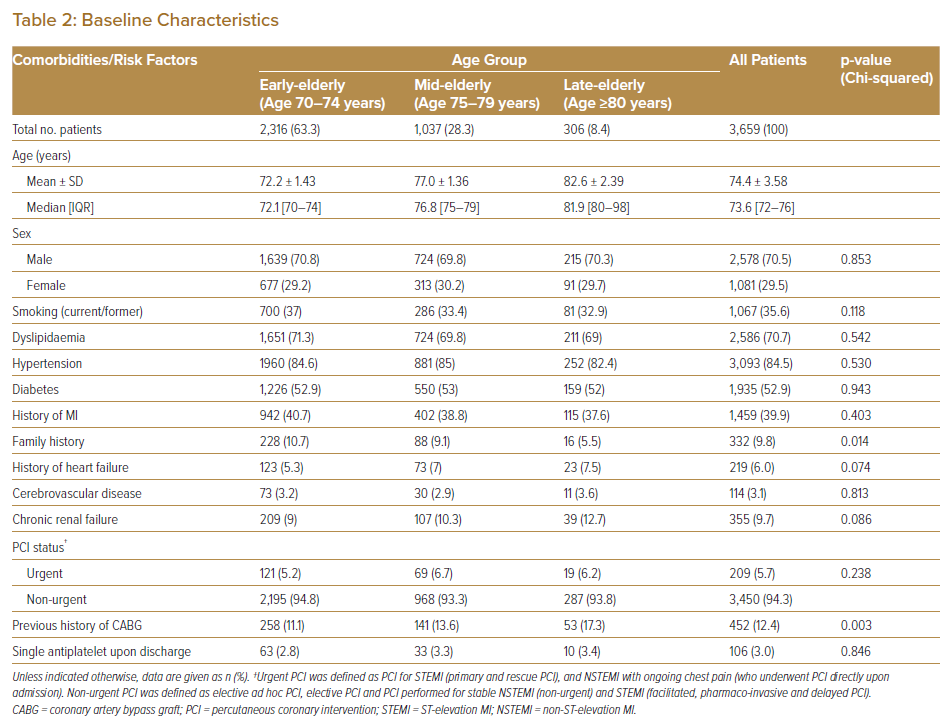
In each age group, the number of elderly patients admitted for PCI increased over time. Overall, the total number of elderly patients admitted for PCI increased from 244 in 2007 to 438 in 2016. Most admissions were from the early-elderly group (n=2,316 [63.3%]; Table 1). The oldest patient enrolled in the study was a 98-year-old man admitted for NSTEMI who underwent successful elective PCI to the mid-left anterior descending (LAD) and left circumflex (LCX) arteries in 2012. Baseline characteristics for each age group are summarised in Table 2. Most patients were male (70%).
The most common comorbidity among the elderly patients who underwent PCI was hypertension (84.5%), followed by dyslipidaemia (70.7%) and diabetes (52.9%); the least common comorbidity was a previous history of stroke (3.1%). Among the entire cohort, 39.9% of patients had a previous history of MI, 6% had heart failure (LVEF <35%) and 9.7% had chronic renal failure, defined as an estimated glomerular filtration rate <60 ml/min/1.73 m2. Most of the patients in this study (94.3%) underwent PCI as an elective procedure; only 209 (5.7%) patients underwent urgent PCI.
The clinical characteristics that differed significantly across the three age groups were a family history of ischaemic heart disease (p=0.014) and a previous history of CABG (p=0.03). Over the 10 years of the study, only 16 of 306 (5.5%) patients aged ≥80 years (late-elderly group) had a positive family history of ischaemic heart disease. This rate was significantly lower than in the early- and mid-elderly age groups (10.7% and 9.1%, respectively). The percentage of patients with a history of CABG was significantly higher in the late-elderly than mid- and early-elderly groups (17.3% versus 13.6% and 11.1%, respectively).
As indicated in Supplementary Table 1, the percentage of patients presenting with unstable angina was significantly higher among the late-elderly group compared with the early- and mid-elderly groups (15% versus 10.7% and 12.9%, respectively; p=0.027). However, there were no significant differences among the three groups for all other types of coronary heart disease. Most admissions (51%) were for chronic stable angina. However, it should be noted that coronary heart disease data were not available in the electronic medical records for 482 (13.2%) patients. There was no significant difference in LVEF among the three age groups.
Supplementary Table 2 details the angiographic findings and procedures undertaken. Of all PCI procedures performed among elderly patients, 92.6% were for de novo coronary lesions; this is statistically significant (p<0.001). Regarding the number of vessels involved, although overall most elderly patients required interventions for single-vessel disease (51.7%), the percentage of patients in the late-elderly group with multivessel disease requiring intervention (55.6%) was significantly higher than in the mid-elderly and early-elderly (49.7% and 46.8%, respectively; p=0.009). However, there was no significant difference among age groups with regard to the coronary artery (i.e. LAD, LCX and right coronary artery) being treated. There was also no significant difference in the type of lesion being treated, although most lesions were Type C lesions (52.7%).
Generally, although fewer left main stem (LMS) vessels (i.e. only LMS and LMS-LAD/LCX bifurcation stenting) were treated in the early-elderly group, the difference did not reach statistical significance. However, rates of provisional LMS-LAD (3.0%) and LMS-LCX (0.7%) stenting were significantly lower in the early-elderly age group than in the mid-elderly (LMS-LAD 4.2% and LMS-LCX 1.5%) and late-elderly (LMS-LAD 4.6% and LMS-LCX 3.0%) groups. One possible explanation for the lower rates of PCI for patients with LMS disease in the early-elderly age group may be that complete revascularisation via CABG is still considered safe in most of these patients compared with patients in the older age groups.
Most lesions treated in this study were ostial lesions (11.0% of all lesions across all age groups), with a significant higher rate of ostial lesions among late-elderly patients compared to early-elderly and mid-elderly (15.2% versus 9.5% and 12.9%, respectively; p<0.001). The next most common lesions were bifurcation lesions (9.5% of all lesions across all age groups). With regard to intracoronary devices, the use of rotablation was significantly higher among the late-elderly group compared with the early- and mid-elderly groups (5.2% versus 3.0% and 4.4%, respectively; p=0.007). This finding is not surprising because vessel calcification is a hallmark of ageing. There were no differences in the types of stents or drug-coated balloons used in elderly patients across the three age groups.
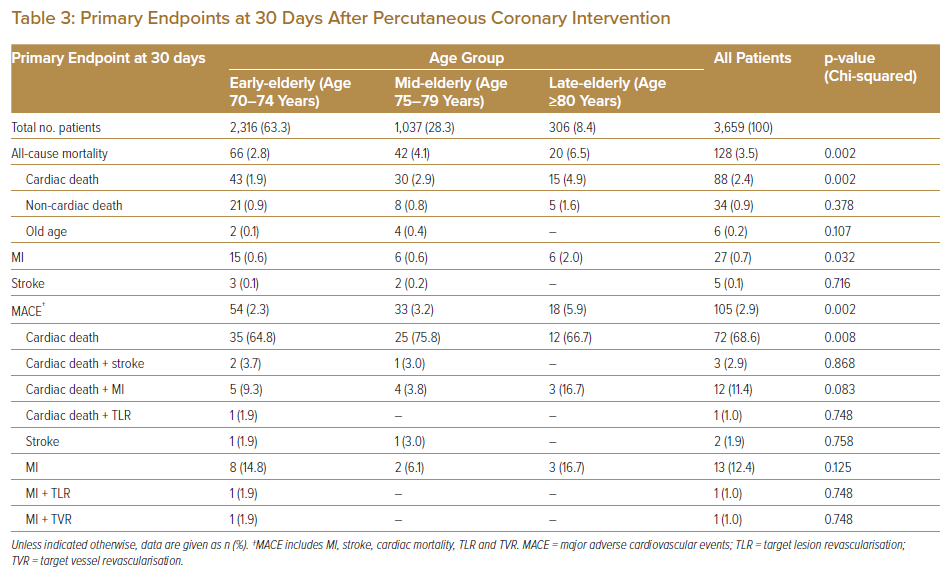
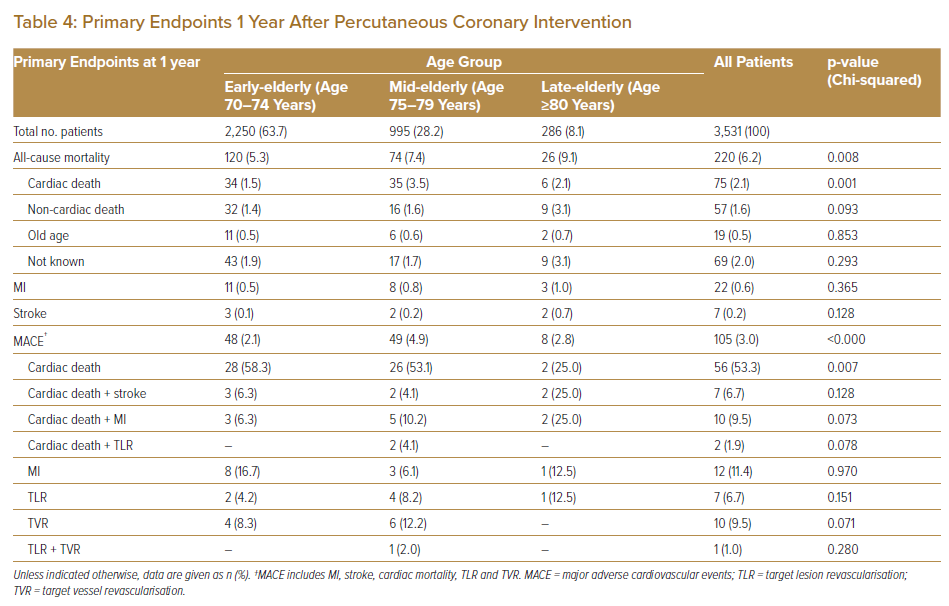
Primary endpoint analysis, summarised in Tables 3 and 4, showed that all-cause mortality at 30 days and 1 year after PCI differed significantly between the three age groups. At 30 days, all-cause mortality was higher in the late-elderly age group than in the early- and mid-elderly groups (6.5% versus 2.8% and 4.1%, respectively; p=0.002). Mortality within 30 days after PCI was mostly related to cardiac deaths. Rates of MI and pure cardiac death 30 days after PCI were significantly higher in the late-elderly population than in early-elderly and mid-elderly (MI: 2.0% versus 0.6% and 0.6%, respectively; p=0.032 and pure cardiac death: 4.9% versus 1.9% and 2.9%, respectively; p=0.002). All-cause mortality at 1 year was also significantly higher in the late-elderly group compared with the mid- and early-elderly groups (9.1% versus 7.4% and 5.3%, respectively; p=0.008). The primary contributor to all-cause death at 1 year was cardiac death in all age groups (Tables 3, 4).
Overall, the risk of MACE within 30 days after PCI was significantly higher in the late-elderly group than in the early- and mid-elderly groups (5.9% versus 2.3% and 3.2%, respectively; p=0.002), with the main contributors being cardiac death (66.7%) and cardiac death associated with MI (16.7%). There were no significant differences in rates of TLR/TVR among the age groups within 30 days after PCI. However, at 1 year after PCI, rates of MACE were significantly higher in the mid-elderly group than in the early- and late-elderly groups (4.9 versus 2.1% and 2.8%, respectively; p<0.001). This was contributed to, in part, by the higher, albeit not significant rate of TVR in the mid-elderly population.
Correlation Analyses Between Clinical Characteristics and Primary Endpoints After Percutaneous Coronary Intervention
Further analyses were conducted to assess correlations between clinical characteristics and both all-cause mortality and MACE at 30 days and 1 year after PCI, as detailed below.
Univariate and Multivariate Analyses at 30 Days After Percutaneous Coronary Intervention
All-cause Mortality
The results of univariate analysis assessing correlations between clinical characteristics and all-cause mortality at 30 days after PCI are summarised in Supplementary Table 3. Significant linear correlations were found for chronic renal failure and urgent PCI status with all-cause mortality in each of the three age groups. Conversely, univariate analysis revealed that only urgent PCI status was linearly associated with MACE 30 days after PCI (Supplementary Table 4).
As indicated in Supplementary Table 5, multivariate analysis revealed that dyslipidaemia (OR 2.4; 95% CI [1.146–4.947]; p=0.02) was associated with higher all-cause mortality at 30 days after PCI in the early-elderly group (age 70–74 years). In the mid-elderly (age 75–79 years) and late-elderly group (≥ 80 years old), although statistically not significant, dyslipidaemia was still associated with higher all-cause mortality at 30 days after PCI (mid-elderly: OR 1.9; CI [0.857–4.411], p=0.111 and late-elderly: OR 2.5; CI [0.783–8.133], p=0.121).
Major Adverse Cardiovascular Events
The results of multivariate analysis of MACE at 30 days after PCI are summarised in Supplementary Table 6. Across all age groups, Urgent PCI status is the significant predictor of MACE. Among patients in the early-elderly group, MACE at 30 days was significantly associated only with urgent PCI status (OR 7.8; 95% CI [4.181–14.638]; p<0.001). Among mid-elderly patients, MACE was significantly associated with chronic renal failure (OR 3.3; 95% CI [1.404–7.935]; p=0.006) and urgent PCI status (OR 14.8; 95% CI [6.934–31.374]; p<0.001). In late-elderly patients, MACE was significantly associated with urgent PCI status only (OR 6.6; 95% CI [1.909–22.896]; p=0.003).
Univariate and Multivariate Analyses 1 Year After Percutaneous Coronary Intervention
Results of univariate and multivariate analyses assessing correlations between clinical characteristics and all-cause mortality and MACE 1 year after PCI are summarised in Supplementary Tables 7–10. Neither univariate nor multivariate analysis for all-cause mortality at 1 year after PCI revealed any specific correlations. Univariate analysis for MACE at 1 year after PCI did not reveal any specific correlations either. However, multivariate analysis for MACE at 1 year post PCI among the early-elderly age group showed significant correlation to dyslipidaemia (OR 2.4; CI [1.052–5.298]; p=0.037) and history of heart failure (OR 2.5; CI [1.030–6.034]; p=0.043). Mid-elderly patients showed MACE correlation in males (OR 3.2; CI [1.361–7.671]; p=0.008). Late-elderly patients showed MACE correlation to chronic renal failure (OR 7.5; CI [1.798–31.402]; p=0.006).
Kaplan–Meier Survival Analysis
Kaplan–Meier survival analysis revealed that the probability of survival at 30 days after PCI was highest for the early-elderly group (97.1%), followed by the mid-elderly group (95.8%) and then the late-elderly group (93.4%; Figure 2; Supplementary Table 11). A similar trend was seen for survival at 1 year after PCI, with the highest survival rate in the early-elderly group, followed by the mid-elderly and then late-elderly groups (92%, 88.9% and 84.9%, respectively).
Discussion
The findings of this study suggest that all-cause mortality and MACE at 30 days and 1 year after revascularisation via PCI increases with age. Overall, revascularisation via PCI in elderly patients (age ≥70 years old) is associated with a mean rate of all-cause mortality at 30 days and 1 year of 3.5% and 6.2%, respectively. The rate of all-cause mortality at 30 days and 1 year after PCI is highest among the late-elderly (6.5% and 9.1%, respectively), followed by the mid-elderly (4.1% and 7.4%, respectively). The early-elderly have the lowest rate of all-cause mortality at 30 days and 1 year after PCI (2.8% and 5.3%, respectively). Overall, the risk of MACE 30 days and 1 year after PCI in elderly patients (age ≥70 years) is 2.9% and 3.0%, respectively. The risk of MACE 30 days after the procedure follows the same trend as seen for all-cause mortality, with the highest risk among late-elderly patients. However, the risk of MACE 1 year after the procedure is highest in the mid-elderly group, with a significant contribution from high rates of TLR/TVR.
The number of patients undergoing urgent PCI was highest in the mid-elderly group, and univariate analysis shows a statistically significant correlation between MACE and urgent PCI. In this study, risk of MACE at 30 days after PCI were significantly higher among patients with urgent compared with elective PCI in all age groups. This finding provides similar prognostic insights as the GUSTO-IIb and PAMI-1 trials and highlights the importance of both early intervention in patients with chronic stable angina and screening for coronary heart disease before a cardiac event happens. Identifying high-risk baseline clinical characteristics, such as those highlighted in the present study, and further investigating or considering early angiograms, as recommended by the TACTICS-TIMI trial, among the geriatric groups, regardless of age group, is crucial.
The PAMI-1 trial demonstrated that the significant reduction in the incidence of recurrent ischaemia and reduced mortality after angioplasty at 6 months (from the PAMI trial) extended to 2 years. Similar observations were made in the present study, but only up to 1 year after PCI. Similarly, there was a reduction in MACE in the group undergoing urgent PCI (involving primary PCI), as well as substantial reductions in readmissions for revascularisation. The observations in the present study were not extended beyond 1 year because the follow-up of most patients was changed to their respective referring hospitals (as per local government policy to reduce overcrowding and to allow for new referrals to tertiary treatment centres).
This study shows that 30 days after PCI, MACE outcomes depend primarily only on urgent PCI status. There was no significant association between MACE 1 year after PCI and any clinical characteristics in any of the three age groups. However, 30 days after PCI, all-cause mortality was highest among patients who had undergone urgent PCI and those with chronic renal failure. At 1 year after PCI, all-cause mortality was correlated with chronic heart failure (among early-elderly group) and renal failure (among late-elderly group).
This principal finding of this study is that intervention in the elderly is tolerated reasonably well, which is comparable to reports from other centres.5–9 Unfortunately, the quality of the available evidence is low, being limited to patient registries. Inevitably, the elderly population is more likely to be vulnerable, hence limiting their participation in trials.10 This restricts the possibility of a randomised controlled trial in this group, and so the present study was designed as a retrospective cross-sectional study.
Elderly patients have more cardiovascular risk factors and are at higher risk of subsequent cardiovascular events with a more severe disease burden (less ischaemic reserve). A less compliant heart (less tolerant to myocardial oxygen supply–demand mismatch) in elderly patients compared with that in younger patients may derive a more significant benefit from revascularisation. In this regard, trials of coronary revascularisation have generally shown that patients at high risk derive more significant benefits from revascularisation than patients at low risk.8,11
The combination of improved patient selection, the evolution of revascularisation techniques, newer stents and the broader use of evidence-based periprocedural medications that balance the risks of thrombosis and bleeding will significantly reduce PCI-associated mortality among the elderly.3,8,11 As the world’s elderly population grows rapidly, so too will revascularisation among the elderly, and the outcome seems promising. Overall, good outcomes following PCI in the elderly are favoured by an elective PCI status and in the absence of chronic renal failure and chronic heart failure.
A potential confounding factor in this study is bias in patient selection for intervention; this is particularly relevant among the elderly population, for whom decisions regarding interventions are based on factors such as frailty, family support and the presence of other debilitating conditions, such as malignancy with poor prognosis. Further studies examining correlations between a frailty index (e.g. based on a clinical frailty scale) with PCI outcomes may further rationalise the basis for the selection of patients for revascularisation intervention.
The main limitation of this study is that we used observational data obtained from institutional electronic medical records and administrative databases. We may have missed post-procedural cardiovascular events among patients living in other Malaysian states, especially if these patients sought treatment at their respective local state hospitals and failed to update their clinicians during subsequent clinic visits. In addition, the data used in this study were for the period 2007–16. Various newer techniques, devices and medicines may have changed the current setting and therefore limit the extrapolation of our findings. Furthermore, we did not consider the effects of the treating physician’s preferences, the patient’s clinical status and the operator’s skill on PCI outcomes. All patients who underwent PCI performed by senior and junior interventional cardiologists, regardless of experience and lesion complexity, were enrolled in the study. More importantly, we enrolled patients on any antiplatelet medication (aspirin, ticlopidine, clopidogrel, prasugrel), those on dual, single or no (high bleeding risk patients) antiplatelet agents and those receiving antiplatelet therapy for any duration (none to maximum dual antiplatelet therapy up to 1 year), although it should be noted that there were no specific data on the use of antiplatelet agents in the electronic medical records. Nevertheless, these last two limitations are advantages for the generalisability of the study findings to the real-world setting.
Conclusion
In conclusion, revascularisation via PCI is safe with acceptable short- (30 days) and mid-term (1 year) outcomes in the elderly population. Immediate outcomes (30 days after PCI) in terms of both MACE and all-cause mortality are better in patients undergoing elective PCI and those without chronic renal failure or dyslipidaemia (only MACE). Mid-term outcomes (1 year after PCI) in terms of all-cause mortality are better in patients without chronic heart failure or chronic renal failure. With the changing demographics of the heart disease patient population leaning towards the elderly, we should focus on appropriate patient selection for revascularisation. Clinicians and patients need to weigh these intervention risks against the significant potential improvement in cardiovascular wellbeing instead of deciding PCI risks based on age alone.
Click here to view Supplementary Material.
Clinical Perspective
- This study investigated the real-world clinical outcomes following PCI (both emergency and elective) in elderly patients.
- The findings provide clinicians with actual risks of PCI in specific age groups to use during angiogram and angioplasty counselling, rather than using an approximate generalised value for all; the actual risk at advanced age is much higher than for the general population.
- Safety from all-cause mortality and MACE at the periprocedural time and up to 1 year after PCI among the elderly population favours those with elective PCI and those without chronic renal failure, dyslipidaemia, or chronic heart failure.