Complications often occur following femoral artery puncture. One of these includes the formation of a femoral artery pseudoaneurysm (FAP), although it has now become less common as trans-radial access has become more popular. Nevertheless, it is important for clinicians to recognise this complication because femoral artery punctures are still widely performed.
We report a novel case of rapid FAP expansion treated using subcutaneous fat embolisation in a resource-limited setting.
Case Presentation
A 61-year-old woman with diabetes, hypertension and end-stage renal failure presented to our emergency department after an episode of angina. She suffered from multiple episodes of recurrent intradialytic hypotension and angina during her regular haemodialysis 2 weeks before. She weighed 98 kg and was 158 cm tall with a BMI of 39.3 kg/m2. High-sensitivity troponin C was markedly elevated (1,854 mmol/l) and her ECG on arrival revealed T-wave inversions in leads I, aVL and V2 to V5.
She was treated for a non-ST-elevation acute coronary syndrome and had coronary angiography performed, which revealed diffuse triple vessel disease with involvement of the left main stem. She was initially referred to the cardiothoracic surgeons, but was deemed high risk following evaluation. Due to her persistent symptoms while undergoing haemodialysis as an inpatient, where she had needed inotropic support, a decision was made to perform percutaneous coronary intervention via femoral artery access. The femoral puncture was performed under fluoroscopic and ultrasound guidance. A 3.0 × 28 mm drug-eluted stent was implanted in the left main artery and left anterior descending artery and a 3.0 × 20 mm drug-eluting balloon was used for the left circumflex artery.
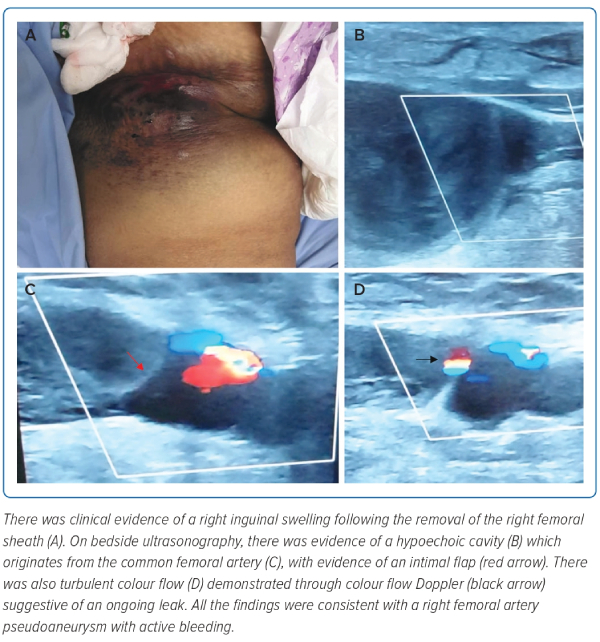
Unfortunately, following removal of her right femoral sheath, the patient became unresponsive. Her vital signs included a heart rate of 120 BPM, blood pressure of 60/42 mmHg, respiratory rate of 28/min, with an oxygen saturation of 92% on room air. Examination revealed a large swelling and bruising of the right femoral area (Figure 1). Alongside aggressive fluid resuscitation and rapid sequence induction for intubation and mechanical ventilation, a bedside ultrasound was performed revealing a hypoechoic cavity originating from the femoral artery, with evidence of an intimal flap and turbulent flow demonstrated on colour Doppler imaging (Figure 1 and Supplementary Video 1). This was consistent with a likely FAP with active leaking and expansion.
A surgical consultation was obtained, but the patient was considered too unstable for another surgical intervention. A decision was made to perform peripheral angiography and intervention to manage the pseudoaneurysm.
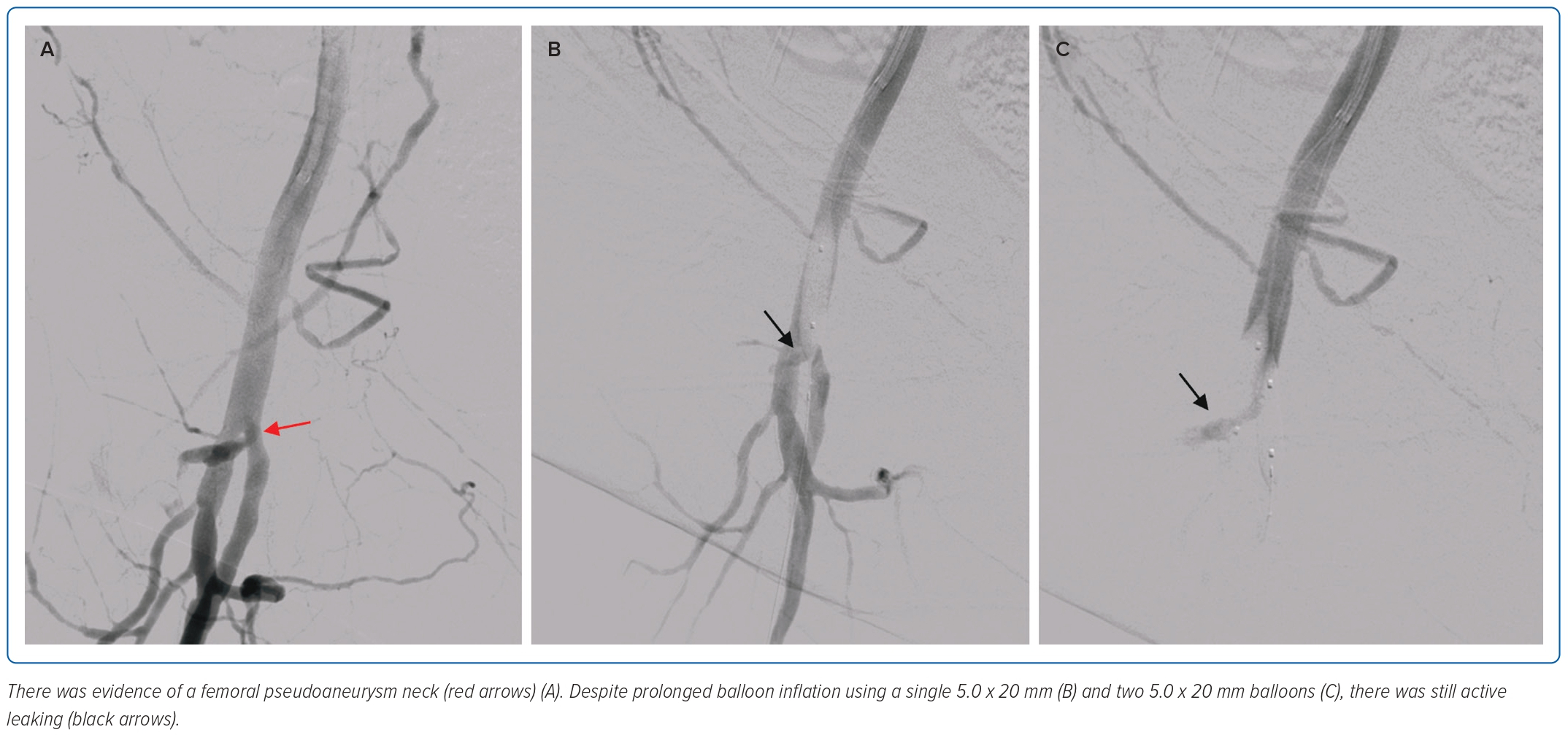
Femoral access was obtained on the contralateral side under fluoroscopic and ultrasound guidance. Initial digital subtraction angiography (DSA) identified the neck of the FAP emerging at the level of the bifurcation of the common femoral artery, leading into the superficial femoral artery (Figure 2).
There were attempts at prolonged inflation using a single 5.0 × 20 mm non-compliant balloon and later two of the same balloons (Figure 2). However, this was unsuccessful. Due to limited resources, there were no balloons of a larger diameter available and similarly there were no embolisation coils or covered stents that were large enough for implantation in the femoral artery.
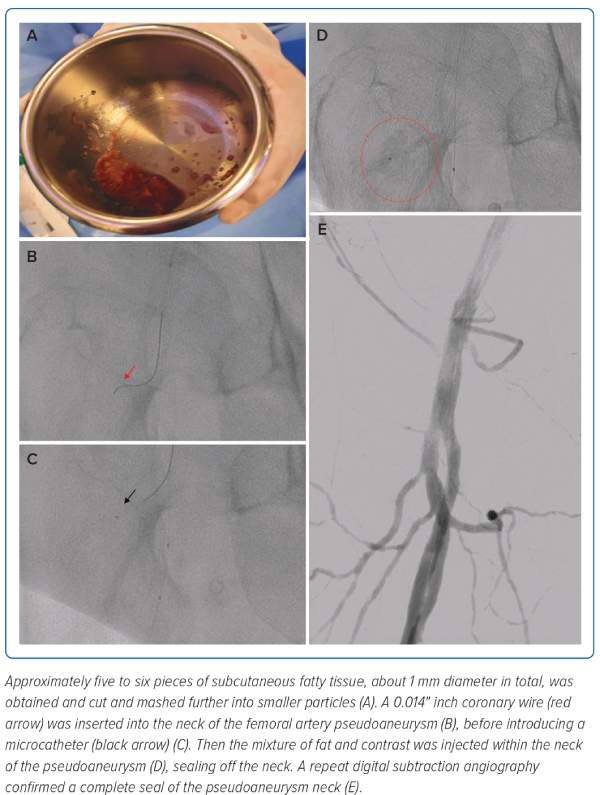
It was decided that subcutaneous fat embolisation, similar to coronary artery perforation management, was worth attempting with subcutaneous fatty tissue being harvested from the patient’s own abdomen (Figure 3). Approximately five to six pieces of subcutaneous fatty tissue – about 1 mm of diameter in total – were obtained and cut and mashed into smaller particles. A 3 ml syringe was filled with the mashed subcutaneous fatty tissue first followed by 2 ml of contrast agent, to form a 2:1 fat:contrast mixture. After this, a 0.014" coronary wire was used to enter the neck of the FAP before introducing a microcatheter into the neck and injecting the fat-contrast mixture under fluoroscopy to ensure controlled amounts of fat-contrast mixture were administered (Figure 3).
Using an over-the-wire balloon would have been an option to avoid simultaneous embolisation of particles when inflated. However, in view of the relatively narrow-necked FAP, we wanted to avoid any unnecessary expansion of the FAP neck and opted for a much smaller microcatheter, which proved sufficient. A repeat DSA confirmed a complete seal of the pseudoaneurysm neck within 1 minute of administration of the fat-contrast mixture (Figure 3 and Supplementary Video 2).
The patient remained stable over the next 48 hours. However, due to prolonged fluid and blood product resuscitation, she developed severe pulmonary oedema, which was difficult to manage through continuous veno-venous haemofiltration due to concurrent severe myocardial stunning. A bedside ultrasound did not show further expansion of the FAP, but she died from her illness 72 hours after the procedure. Unfortunately, due to persistent fluid overload and worsening heart function from the prolonged insult prior to the fat embolisation, she could not recover.
Discussion
Complications of femoral artery access include dissections, occlusion, embolisation, arterio-venous fistula formation, pseudoaneurysms, bleeding at the access site or retroperitoneally. The presence of an intimal flap and ‘neck’ would be highly suggestive of pseudoaneurysm formation. Usually, this is best assessed either with ultrasonography or CT with angiography of the femoral artery.1,2
FAP is a known complication that follows femoral artery access. The recorded estimated prevalence following coronary angiography (0.1–0.2%) and percutaneous intervention (0.8–2.2%) may be outdated as the radial artery has since become a preferred route of access for such procedures.1
Common risk factors include older age, obesity, being a woman, hypertension and the puncture site being lower or at the distal end of the common femoral artery.2 All these risk factors were present in this patient. Pseudoaneurysms often progress due to sustained arterial pressure, causing blood to dissect into the tissues around the damaged artery and form perfused sacs with communication into the arterial lumen.1,2 Although some FAP undergo spontaneous thrombosis, others require intervention.
Management normally depends on the haemodynamic status of the patient. Stable patients are often managed through ultrasound-guided compression or ultrasound-guided thrombin injection.1–3 Traditionally, haemodynamically unstable patients may warrant surgical intervention when available.1–4 However, endovascular intervention including prolonged balloon inflation, use of stents or grafts, and embolisation coils have also been successful as reported in the literature.5 However, there has not been a similar case of FAP reported and managed using subcutaneous fat embolisation, despite it being commonly performed after coronary artery perforation.6–8
Subcutaneous fat is an effective embolisation tool as it can obstruct the intended lumen of the perforated artery and it contains fibroblast cells and fat cells, which contain a lot of tissue factors that help to initiate the extrinsic coagulation pathway during traumatic vascular injury.7 The risk of migration of fat particles, although theoretically plausible, is relatively low when dealing with coronary arteries. However, the common femoral artery is a large and proximal artery and therefore risk of embolisation would have been higher when trying to perform fat embolisation. Therefore, it was essential that we used a microcatheter to deliver a controlled amount of fat-contrast mixture into the neck of the pseudoaneurysm.
Conclusion
Although surgical intervention remains an important aspect of management in haemodynamically unstable pseudoaneurysm expansion, percutaneous interventions provide a reasonable alternative, especially in cases where surgery is not feasible. Our case report highlights how subcutaneous fat remains a viable option as a material if embolisation is attempted, especially in a setting with limited resources. 
Clinical Perspective
- There is limited role for vascular ultrasound-guided compression in a haemodynamically unstable patient with femoral pseudoaneurysm.
- Ideally, the catheterisation laboratory should be equipped with essential tools such as peripheral balloons and stents or embolisation coils to overcome complications related to femoral artery vascular access.
- When embolisation is attempted, subcutaneous fat remains a viable alternative when options are limited, as in our case.