Ageing of the global population is a significant demographic megatrend, which has led to an increased incidence of cardiovascular disease, specifically coronary artery disease.1,2 With the prevalence of chronic total occlusion (CTO) reported as high as 30% in angiographic databases, the disease burden of CTO is substantial.3 Owing to the complexity of elderly patients, who frequently have multiple comorbidities and frailty, the elderly population less frequently undergoes revascularisation for their coronary artery disease, especially CTO.2–4 This is due to previous reports indicating that advanced age is associated with higher rates of complications related to percutaneous coronary intervention (PCI) and worse major adverse cardiac events (MACE) outcomes when compared to younger adults.2–4 Given the higher risk of complications associated with coronary artery bypass graft surgery (CABG) and PCI in this vulnerable patient group, medical therapy is often implemented despite the potential benefit of revascularisation.4
Recent advancements in CTO-PCI techniques and devices, including dedicated guidewires and microcatheters, have improved the success rate and safety of CTO-PCI procedures.2,4 However, the available data on CTO-PCI outcomes in elderly patients are limited, with less than 10 studies published.2 Therefore, we aimed to investigate the feasibility, safety and clinical outcomes of CTO-PCI in elderly patients aged <75 years versus ≥75 years in a high intravascular imaging usage centre.
Methods
Study Population
A retrospective analysis was conducted on 258 patients who underwent at least one CTO-PCI at Okamura Memorial Hospital, Shizuoka, Japan, from September 2015 to April 2021 via the electronic health record. Patients were categorised as either <75 years old or ≥75 years old. Demographic, clinical, angiographic and peri-procedural information, as well as in-hospital and long-term outcomes were analysed. Indication for CTO-PCI was the presence of angina, heart failure and/or inducible ischaemia. Follow-up data were obtained from the hospital’s electronic health record.
Treatment Strategy
All CTO-PCIs were performed by highly experienced Japanese CTO-PCI specialists certified by the Japanese Board of CTO Interventional Specialists. The revascularisation strategy – either antegrade, retrograde, or hybrid approach as previously described – was selected at the operator’s discretion.5 Activated clotting time was monitored throughout the procedure and kept above 250 seconds. Most cases were performed with dual vascular access, and contralateral contrast injection was performed to assess the CTO lesion unless ipsilateral collateral CTO was present. Vascular access was secured with a vascular closure device post-procedure, and dual-antiplatelet therapy was prescribed according to local guidelines.6
Definition and Outcomes
A CTO was defined as the obstruction of a native coronary artery with a Thrombolysis in MI (TIMI) flow grade 0 for more than 3 months clinically.3 The duration was estimated based on the interval from the last episode of the acute coronary syndrome or, in patients with no history of acute coronary syndrome, from the first episode of exertional angina consistent with the location of the occlusion or previous coronary angiography. Successful CTO-PCI was defined as successful CTO revascularisation, achieving less than 30% residual diameter stenosis within the treated segment and restoration of antegrade TIMI grade 3 flow.
The primary outcome was target lesion failure (TLF) during a 1-year followup. TLF was defined as a composite of cardiac-related death, target vessel non-fatal MI, and clinically driven target lesion revascularisation (TLR) as per the Academic Research Consortium-2 definition.7 All deaths were considered cardiac in origin unless a definite non-cardiac cause was established.7
Statistical Analysis
Categorical variables were expressed as frequencies and percentages. Continuous variables were described as mean and standard deviation for normally distributed variables or median and interquartile range for nonnormally distributed variables. The normality of numerical data was assessed using visual inspection of histograms and the Shapiro–Wilk test. The χ2 test or Fisher’s exact test was used for categorical variable comparisons, while the Student’s t-test or Mann–Whitney rank-sum test was used for continuous variables, as appropriate. The Cox regression method was used to estimate survival free from TLR, and the log-rank test was used to compare survival curves. Multivariable Cox regression analysis was used to identify predictors of TLR in patients aged 75 years or older. Survival curve analysis was performed with the Kaplan-Meier curve and compared with the log-rank test. Univariable logistic regression was performed to determine associations between variables and TLF. Variables with a p value <0.05 in univariable analysis and those considered clinically and angiographically plausible predictors of TLF were included in multivariable logistic regression with sensitivity analysis. Statistical significance was set at p<0.05 for multivariable analysis. The effect of a particular variable of interest on 1-year TLF was expressed as an OR with a 95% CI. The statistical analysis was conducted using IBM SPSS version 26 (SPSS).
Results
Baseline Clinical Characteristic
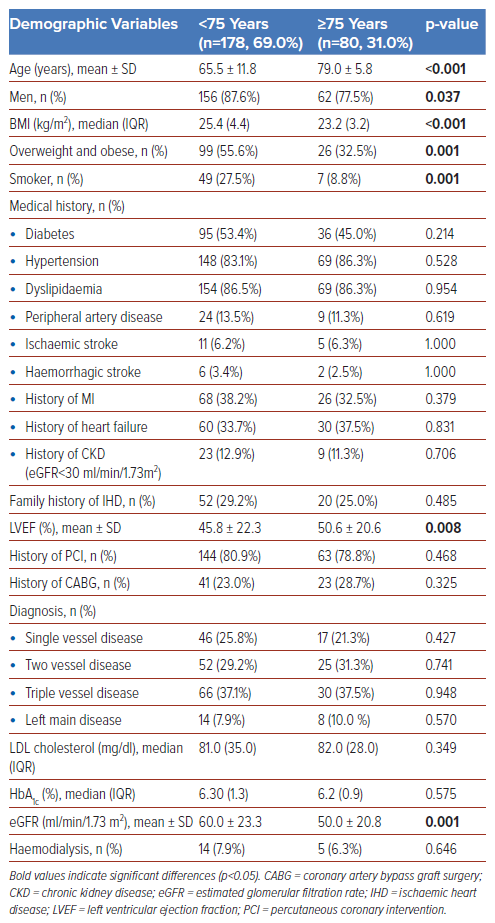
The study population consisted of 258 subjects who underwent CTO-PCI between September 2015 and April 2021. The population was stratified into two age groups: younger elderly (<75 years old) and older elderly (≥75 years old). The demographic characteristics of the population are summarised in Table 1. Of the population, 178 (69.0%) were in the younger elderly group, and 80 (31.0%) were in the older elderly group. Significantly more men were in the younger elderly group (87.6% versus 77.5%, p=0.037), as were individuals with higher BMI (25.4 versus 23.2, p<0.001), higher rates of overweight and obesity (55.6% versus 32.5%, p=0.001), and higher rates of smoking (27.5% versus 8.8%, p=0.001). Left ventricular ejection fraction (LVEF) was significantly lower in the younger elderly group compared to the older elderly group (45.8% versus 50.6%, p=0.008). However, the estimated glomerular filtration rate was lower in the older elderly group compared to the younger elderly group (50.0 versus 60.0, p=0.001). There were no statistically significant differences in other parameters between the two age cohorts, including medical history, family history, history of PCI or CABG, diagnosis of coronary artery disease, and blood investigations.
PCI Details
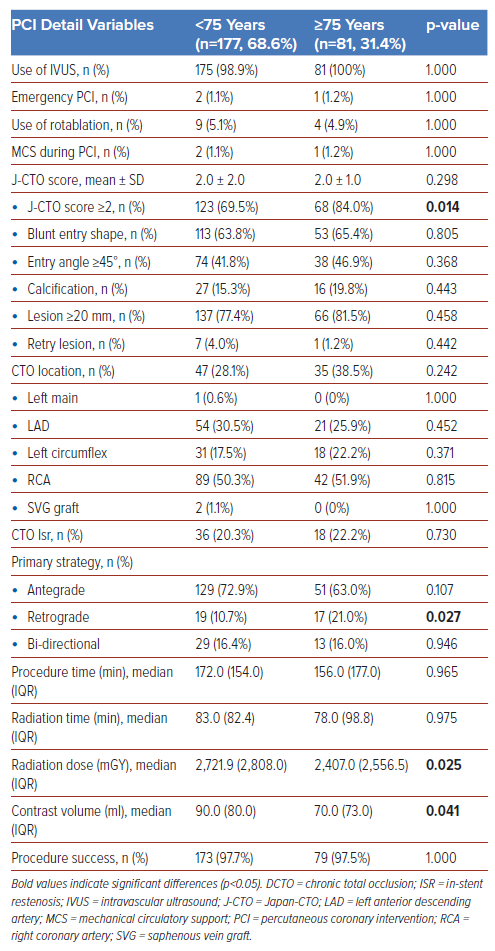
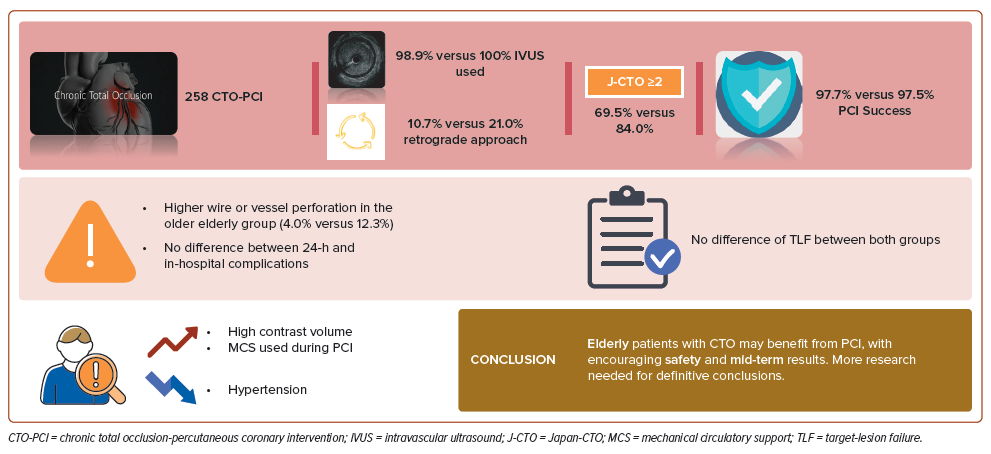
Regarding the CTO-PCI procedure, both age groups showed high use of intravascular ultrasound, with reported rates of 98.9% in the younger elderly group and 100% in the older elderly group. The older elderly group had a higher proportion of subjects who underwent retrograde wiring strategy (10.7% versus 21.0%, p=0.027). Our study showed no statistically significant differences between the two age groups in patients who underwent emergency PCI for acute coronary syndrome, rotablation, use of MCS during CTO-PCI (in line with the Japanese Circulation Society guideline), CTO vessel location, in-stent restenosis (ISR) in CTO-PCI, procedure time, and radiation time.8 The younger elderly group had higher radiation dose (2,721.9 mGy versus 2,407.0 mGy, p=0.025) and contrast volume (90.0 ml versus 70.0 ml, p=0.041). Although the older elderly group had a significantly higher proportion of difficult lesions with Japan-CTO (J-CTO) score ≥2 (69.5% versus 84.0%, p=0.014), both age groups achieved a similarly high CTO-PCI procedural success rate (97.7% versus 97.5%, p=1.0). All the details are summarised in Table 2 and Supplementary Figure 1.
Complications, Follow-up and Outcomes
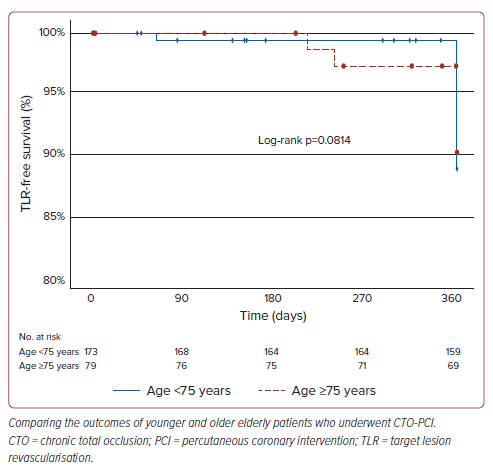
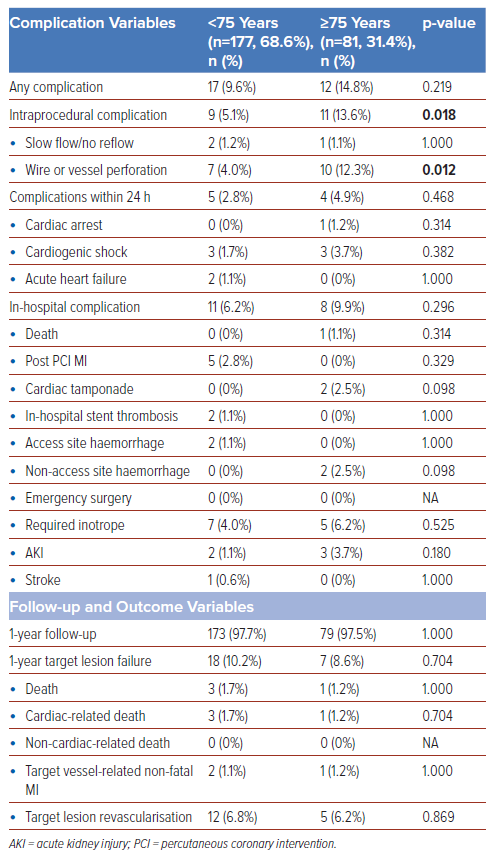
The complication, follow-up, and outcome variables are summarised in Table 3. There was a significantly higher rate of intraprocedural complications in the older elderly group compared to the younger elderly group (5.1% versus 13.6%, p=0.018), mainly due to wire or vessel perforation (4.0% versus 12.3%, p=0.012). However, the two groups had no significant differences in 24-hour or in-hospital complications. Of the attempted CTO-PCI procedures, 173 (97.7%) of the younger elderly group and 79 (97.5%) of the older elderly group completed the 1-year follow-up. There were no significant differences between groups in 1-year TLF, target vessel non-fatal MI, TLR and death, despite the higher intraprocedural complication rate in the older elderly group. The TLF rates were 10.2% and 8.6% in the younger and older elderly groups, respectively, but the difference was insignificant. Kaplan-Meier survival analysis showed the mean TLF-free survival time for younger elderly was 363.24 (SE 1.81) and 363.24 (SE 2.77) days at the end of the 1-year follow-up. Log-rank analysis showed no significant difference in mean TLF-free time between both groups with a p value of 0.814. This is demonstrated in Figure 1.
Cox-regression analysis in Supplementary Table 1 showed that the use of MCS during PCI (OR 4.91–1,600.35; p=0.002) and emergency PCI (OR 1.004–1.039; p=0.017) were associated with poorer TLR-free survival in the older elderly group compared to the younger elderly group. Hypertension appeared protective, with an OR of 0.009–0.347; p=0.002. The results are summarised in Figure 2.
Discussion
The ageing population poses a significant global challenge, particularly in advanced countries, such as Japan, where projections indicate that individuals aged 75 years and older will constitute over 30% of the population by 2060.1,9 Elderly individuals have a higher burden of medical comorbidities, rendering them more susceptible to age-related issues such as frailty, cognitive impairment and decreased functional capacity.10,11 Additionally, due to their decreased physiological reserve and increased susceptibility to stressors, this group of patients is more vulnerable to adverse outcomes during the PCI, including periprocedural bleeding and contrast-induced nephropathy.2,4,11,12
Furthermore, ageing is a well-established risk factor for ischaemic heart disease (IHD), with significant IHD cases attributed to CTO.3 However, our study showed no difference in medical history between the two groups, although higher BMI and more smokers were observed in the younger elderly group, consistent with the other reports.2,4,11,12 The older elderly group also had a lower estimated glomerular filtration rate but higher LVEF than the younger elderly group.
Over the past few years, PCI, particularly CTO intervention, has advanced due to the development of newer wiring and lesion-crossing techniques, vascular access, and closure devices, CTO-dedicated devices, and improved management algorithms. The European Society of Cardiology recommends CTO-PCI as a class IIA indication for patients with suitable anatomy and those with angina resistant to medical therapy or a large area of documented ischaemia in the territory of the occluded vessels.13 However, the latest American College of Cardiology guidelines gives CTO-PCI a class IIb indication, stating that the benefit of PCI to diminish symptoms is uncertain, especially after treatment of non-CTO lesions in patients with refractory angina on medical therapy, as shown in the DECISION-CTO trial.14,15 The DECISION-CTO trial’s underpowered nature and high crossover rate created uncertainty regarding the symptomatic improvement benefits of CTO-PCI.15 Consequently, until the results of larger trials, such as the NOBLE-CTO and ISCHEMIA-CTO trials, are published, the EUROCTO trial’s symptomatic improvement benefits should be the primary indication for CTO-PCI.16
Despite the challenges associated with performing CTO-PCI in elderly patients, recent studies and meta-analyses have shown that it is feasible, safe, and significantly improves long-term outcomes in successful CTO revascularisation comparable to younger patients.2,4,17–19 One of the major strengths of our study is the extensive use of intravascular imaging, particularly IVUS, during CTO-PCI, with usage rates of up to 98.9% and 100%, respectively. Previous studies and meta-analyses have consistently demonstrated the beneficial effects of IVUS in improving short-, mid-, and long-term clinical outcomes and reducing MACE, even in complex lesions such as CTO.20–27
Our study is unique in that it is the first to compare outcomes between younger and older elderly individuals undergoing CTO-PCI at a centre that extensively uses IVUS. This novel contribution to the literature is important, given that previous research has not investigated this specific comparison to the same extent.2,4,12 However, the lack of a control group without IVUS limits conclusive claims about its specific impact. Future studies directly comparing IVUS and no-IVUS use in our setting could further elucidate its role in this population.
In addition to facilitating optimal stent sizing and expansion, IVUS also plays a critical role in guiding antegrade or retrograde re-entry, controlled antegrade and retrograde tracking (CART), and the reverse-CART technique, as well as in enabling 3D tip detection using newer technology, such as the AnteOwl IVUS (Terumo).25–28 Through the synergistic combination of expert CTO operators, advanced equipment and techniques, and extensive use of IVUS, we achieved remarkably high procedural success rates of 97.7% and 97.5% in both groups.
The older elderly group in our study had a higher proportion of complex CTO cases, as evidenced by more subjects with J-CTO ≥2. This may explain the higher usage of the retrograde approach as the primary strategy in CTO-PCI, which may have led to a higher rate of wire or vessel perforation in the older elderly group. Despite this, there was no significant difference in 24-hour or in-hospital outcomes between both groups and no difference in 1-year TLF, demonstrating the safety and feasibility of CTO-PCI in older elderly patients. This contrasts with previous studies that reported higher in-hospital complication rates and lower technical success in older elderly patients.2,29 We believe that the difference in outcomes may be multifactorial, as discussed previously, and may also be attributed to the high utility of intravascular imaging.
It is imperative to note that while performing CTO-PCI in older elderly patients, appropriate patient selection and attention towards reducing contrast volume are crucial due to the independent risk factor of MACE, as demonstrated in our study. Notably, our study revealed that MCS during PCI and emergency PCI were linked to poorer TLR-free survival in the older elderly group compared to the younger elderly group. Further review revealed that all three patients who required MCS during CTO-PCI did so due to cardiogenic shock. The use of MCS in these cases was in line with the recommendations of the Japanese Circulation Society guideline.8 This observation implies that MCS in older elderly patients warrants careful consideration and may require more prudent management to avert adverse outcomes. These findings align with previous studies indicating a higher complication rate associated with using MCS in CTO-PCI, further highlighting the significance of appropriate MCS use in this patient population.30 Given the observed association between MCS use and poorer outcomes in older elderly CTO-PCI patients, future research should prioritise defining optimal protocols for MCS usage and developing targeted risk mitigation strategies. This could pave the way for safer and more effective interventions in this complex patient group.
In contrast, hypertension seemed to confer a protective effect against TLR in the older elderly group compared to the younger elderly group. These findings are consistent with prior research demonstrating a J-shaped relationship between blood pressure levels and cardiovascular outcomes in elderly patients.31,32 Therefore, the optimal blood pressure target for older elderly patients undergoing CTO-PCI may differ from that of younger elderly patients and necessitate personalised management.
Limitations
Our study has several limitations. First, its retrospective nature and single-centre design, along with a relatively small sample size of Japanese patients, restrict the generalisability of our findings to broader populations and more diverse ethnicities, where CTO characteristics and responses to PCI may differ. Moreover, the follow-up period was not extensive enough to comprehensively assess long-term safety and survival outcomes. Additionally, the specific expertise of the PCI operators at our centre, consistent with published studies, potentially influenced the outcomes and safety of CTO-PCI. This highlights the need for future studies in broader settings with varied operator skill levels to ensure generalisability.33,34 Finally, the lack of a control group comparing intravascular imaging-guided CTO-PCI with angiographically guided-PCI limits us from drawing definitive conclusions about the specific benefit of IVUS in elderly CTO-PCI patients. Future research should include a larger, multicentre randomised controlled trial with longer follow-up to address the limitations to provide more generalisable conclusions about the safety and efficacy of CTO-PCI in elderly patients, particularly focusing on the potential role of intravascular imaging guidance in this specific population.
Conclusion
Our study conducted at a high intravascular imaging usage centre demonstrated no significant differences in feasibility, safety, and mid-term outcomes of CTO-PCI among elderly patients aged <75 and ≥75 years. These findings highlight the potential role of CTO-PCI as a treatment option for carefully selected elderly patients, especially considering the observed safety and good mid-term outcomes in our setting. Additionally, our study identified potential risk factors for MACE and complications, which may inform future management strategies.
Clinical Perspective
- This study demonstrates the feasibility and safety of chronic total occlusion-percutaneous coronary intervention (CTO-PCI) in elderly patients (both <75 and ≥75 years old), potentially expanding treatment options for this previously under-represented population.
- Identification of potential risk factors (mechanical circulatory support, emergency PCI) allows for the development of personalised management strategies to improve outcomes in elderly patients.
- These findings support the potential for CTO-PCI to improve mid-term clinical outcomes in appropriately selected elderly patients, ultimately contributing to enhanced patient care.