Indonesia is experiencing a rapid transition towards chronic noncommunicable diseases, with cardiovascular disease (CVD) being a leading cause of mortality. In Indonesia, CVD contributes to one-third of deaths, with stroke and ischaemic heart disease being the most common causes.1 Patients with ischaemic heart disease have a higher predisposition to premature death, acute coronary syndrome and rehospitalisation. Therefore, international guidelines have emphasised the need for both primary and secondary prevention strategies for CVD.2
In CVD prevention, primary prevention focuses on individuals without preexisting CVD. Many associated risk factors are modifiable, while others have a genetic basis. High blood pressure, diabetes and smoking are among the most prevalent risk factors. The most cost-effective intervention is smoking cessation, and implementing cessation programmes, such as nicotine replacement therapy, has been found to assist 80% of smokers in quitting. Additionally, weight is strongly linked to CVD, making weight management and adopting a healthy diet essential. A diet rich in whole grain products, vegetables, fruits and fish while limiting saturated fats is recommended for optimal cardiovascular health.3
Secondary prevention, in the form of cardiac rehabilitation (CR), is an evidence-based intervention proven safe and effective in reducing morbidity and mortality rates in adults with ischaemic heart disease, heart failure or those who have undergone cardiac surgery. Recent studies show that cardiac secondary prevention is not only clinically effective, but also cost-effective compared with other medical interventions in ischaemic heart disease patients. Ades et al. demonstrated that CR is more cost-effective after MI compared with lipid, thrombolytic and coronary artery bypass graft surgery (CABG) drugs.4 Only smoking cessation was found to be more cost-effective than CR.
A study by Levin et al. in Sweden showed that CR participation after MI or CABG surgery reduced rehospitalisation from 16 to 11 days, increasing the rate of return from 38% to 53% within 5 years.5 Another study by Oldridge et al. indicated that 12 weeks of CR participation reduced medical costs after a follow-up period of only 21 months.6 However, only a fraction of patients were referred to the programme due to various barriers. In response, physicians are exploring alternatives, such as home- or community-based CR.7 In low- to middle-income countries, such as Indonesia, successful implementation of CR has been limited due to factors, such as a shortage of cardiologists and physical infrastructure constraints. There were only approximately 1.5 cardiologists per 1,000,000 population.8
Digital platforms could transform CR and preventive cardiovascular care by enabling remote monitoring, telemedicine and personalised interventions, increasing adherence through mobile apps and wearables. Educational content, behaviour change support and online communities can be used to enhance patient engagement.9 The scalability of digital solutions can also improve accessibility and uptake rates, particularly in acute hospital settings, by eliminating travel constraints and offering relatively more flexible scheduling. An effective digital CR solution should combine wearable monitoring, tailor-made exercise plans, and guidance on diet and lifestyle, aiming for sustained commitment by providing assistance in behavioural change. This can be achieved through community engagement, support and using data-driven tools to track progress, ultimately enhancing the management of cardiovascular health.10
Digitisation of healthcare is seen as a crucial step towards achieving the United Nations’ Sustainable Development Goals. The Ministry of Health in Indonesia is working on a strategy to achieve a Healthy Indonesia in collaboration with the United Nations Development Programme, with funding from Japan.11,12 Pressure from COVID-19 drove demands for telemedicine and catalysed the emergence of effective telehealth methods, both in Indonesia and globally.
Local and government health-related applications have been developed, but health data are highly diverse, fragmented and scattered. Data exchange and standardisation still lack proper regulations. The emerging digital health ecosystem presents a range of opportunities for the business, information and communication technology, and health sectors, as well as investors. However, most importantly, it provides opportunities for Indonesia to learn from the experiences of experts in other countries.
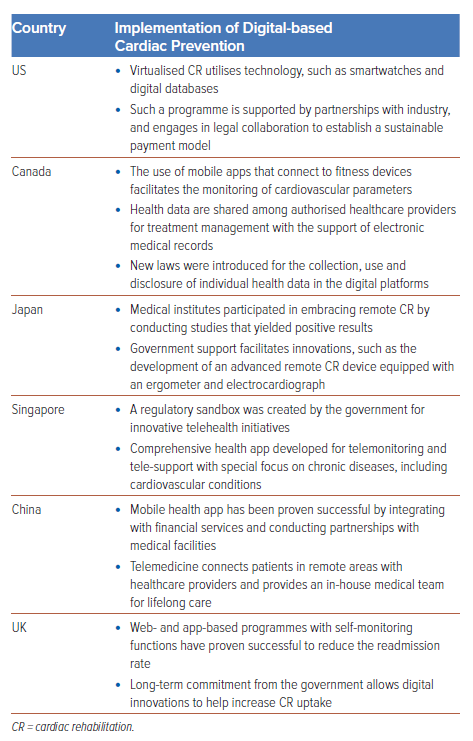
Innovations in Different Countries
Most mobile health applications are targeted for specific diseases worldwide. In 2015, about one-third of mobile health apps were dedicated to mental health, followed by diabetes and CVD. In preventive cardiology, mhealth allows rehabilitated cardiac patients to perform CR programmes from anywhere and at any time they prefer. The effectiveness CR through telemedicine was first identified in 2000 through telephonic monitoring.13 Since then, the evidence is going through a surge, with various methods of delivery and some with mixed results. Adherence of patients was proven to be 1.4-fold higher when CR was performed through the use of mobile applications.14 Meta-analyses of telehealth intervention in secondary prevention of CHD demonstrated lower rates of hospitalisation and cardiac events, as well as better control of blood lipids and smoking cessation in favour of intervention group.15 In this section, we aim to review digital technology’s unique services for CR in different countries (Table 1).
US and Canada
Virtual cardiac rehabilitation programmes, such as the Corrie Health Project at Johns Hopkins, Baltimore, US, and the Central East Cardiac Rehabilitation Programme in Toronto, Canada, improve patient outcomes and empower patients to take charge of their recovery. These programmes use technology, such as smartwatches, pressure cuffs and digital databases, to monitor patient information. To accelerate widespread use in clinical practice, partnerships with industry and the field of law are sought to create a sustainable payment model.16 A similar model was adopted in Toronto, where a centrally managed and regional healthcare team of Central East Cardiac Rehabilitation Programme made a rapid transition from a region-wide, community-based CR to virtual content due to the COVID-19 lockdown. The healthcare team executed e-visits by telephone, email, web-based video supposed and mobile apps. During the study period, increased total referrals of 33% and attendance rate of 85% were seen, and patient satisfaction did not decline.17
Japan
In Japan, only 3.8% of medical institutes could provide remote monitoring of CR after the COVID-19 pandemic hit, and one study showed lower emergency readmission rates within 30 days of discharge and higher quality of life.18 Bi-weekly telephone consultations and weekly CR meetings were conducted. Easy monitoring of blood pressure, ECG and oxygen saturation enabled advanced remote CR, even in elderly patients.18 The Japanese Ministry for Health, Labour and Welfare has been putting further research into developing a stand-alone device specifically to tackle the problem of remote CR. The RH-01 device (Remohab) included an ergometer and ECG for biometric assessment, while online consultation is conducted through a smartphone app.19
UK
Several major trials in the UK investigating mhealth-based CR have provided positive evidence on acceptability, feasibility and efficacy of home- or community-based CR. Web- and app-based programs with selfmonitoring functions were explored to support the work of healthcare professionals. The National Health Service Long Term Plan set a goal to achieve an 85% uptake rate of CR through additional use of digital innovations while still working towards patients’ goals. This is predicted to prevent 23,000 premature deaths and 50,000 acute admissions over 10 years, saving future healthcare related-costs. In 2013, University Hospitals of Leicester NHS Trust developed a website, Activate Your Heart, to increase access to CR for patients with coronary heart diseases. The project had been successful with overwhelmingly positive outcomes, such as increase uptake and completion of the CR programme, 50% reduction of hospital readmission rate, and better patient awareness and knowledge of their cardiac conditions and how to cope.20
Future Directions in Primary Care
The delivery of healthcare services to cardiac patients is relatively accessible and easily accessible. However, in Indonesia, there is a need for equitable healthcare coverage and primary prevention programmes to address chronic diseases, which have a negative prognosis and significant economic impact.21 While local medical applications, such as HaloDoc, Alodokter and GrabHealth, offer virtual consultations, there are currently no apps specifically targeting primary prevention. Using digital health technologies, such as mobile applications, text messaging, wearable sensors and online counselling, can promote healthy lifestyles and behavioural change, particularly in relation to poor diet, smoking and sedentary lifestyles. To successfully implement this vision, a governmentbased mhealth system that is centrally regulated and integrated is necessary. The PeduliLindungi app (now SatuSehat) developed by the Ministry of Health for monitoring the spread of COVID-19 serves as a promising example of such an integrated mhealth system. Successful implementations of digital health technology in primary care in other countries can provide valuable insights and serve as models for Indonesia.
Singapore
The Ministry of Health in Singapore launched a regulatory sandbox to support innovation, and mediate relationships between telehealth partners and the government even before the COVID-19 era. There are 11 start-ups in the sandbox, including MyDoc, DoctorAnywhere and MediSave. Patients eligible for the Community Health Assist Scheme offered by the Ministry of Health can use services through MediSave, which specifically caters to patients with chronic diseases; for example, CVDs, who have undergone physical consultations, while MyDoc provides a comprehensive service for general health, and integrated prevention and management of chronic diseases.22 An extensive network with health partners in Singapore means that those with or at risk of cardiovascular disease can even consult with the insurance agent, local pharmacist and access their laboratory results prior to consultation. The app also allows tracking of health data manually or automatically from a variety of sources, including health screenings and tracking devices. To facilitate telemonitoring and tele-support, the app includes tools using artificial intelligence (AI), where users can be advised on their next course of action based on the list of symptoms they experience.23 As part of a wider comprehensive health support plan, 20,000 pulse oximeters were distributed, and tele-kiosks were made available for video consultations.24 These apps are monitored by the regulatory body, the Health Science Authority, which issues regulatory controls surrounding medical devices.
China
In China, telemedicine is tightly regulated under the National Health Commission and the National Administration of Traditional Chinese Medicine, with strict policies and resources in place. Commercial e-healthcare companies are not permitted to provide services independently and can only collaborate with licensed medical institutions. A collaboration agreement, addressing data privacy concerns, must be reviewed by the local healthcare regulator. Ping An Good Doctor, the largest online healthcare platform in China, offers virtual consultations, hospital referrals, health management services and connects individuals with healthcare resources. It has expanded to provide in-house medical teams for lifelong care in scenarios such as cardiovascular health and disease management. The wider Ping An Group has integrated financial services, corporate health insurance plans and internet hospital platforms in 205 hospitals across 10 cities. This platform connects online and offline services, combining extensive medical resources with influential public hospitals, and providing comprehensive diagnostic and treatment services for cardiovascular patients in remote areas.25
Canada
Telehealth services vary across states in Canada. One telehealth service provider under the direct supervision of the government of Alberta and Alberta Health Services is MyHealth Records mobile app. The goal when developing this app was to create a trusted source of health information and tools for citizens, empowering them to track and monitor health, including immunisations, laboratory test results, vital signs, blood sugars, insulin and medical appointments. It connects to fitness devices for therapeutic activities (e.g. cardio exercises). This benefits individuals with cardiovascular disease risk factors, allowing them to monitor and gain some control over their risks. These data can be made available directly to healthcare providers and pharmaceutical information networks across the province for managing treatments.
To support the framework of networked and integrated health information systems, Alberta Electronic Medical Records provides shared access among authorised custodians to health information in a secure environment. Alberta Electronic Medical Records continues development to realise their vision of ‘one person, one record’. In pursuit of this vision, key initiatives include shared health records, allowing patient information from local clinics to be added to the existing database in Netcare Portal. Netcare transcribes reported data, notifying physicians of changes, which can then be downloaded into local electronic medical record systems in clinics or hospital facilities. Privacy Impact Assessment was introduced under the Health Information Act to regulate newly implemented administrative practices and information systems related to the collection, use and disclosure of individual health data.26
Digital-based Cardiac Prevention in Indonesia
Like many other countries during COVID-19, Indonesia was forced to quickly develop a digital health system in response to the crisis. This has resulted in both the government and the private sectors to further push for a digital transformation for healthcare. Meanwhile, Indonesia is facing an aging population, a growing prevalence of CVD and its comorbidities, the development of costly clinical innovations, and an increasing patient awareness, knowledge and expectation. Disruptive innovation, such as digital cardiovascular preventive care, rather than a traditional approach, seems to be the way forward to tackle the issue. Implementing it, however, will be met with huge obstacles.
To achieve a successful digital cardiac prevention, Indonesia must address challenges posed by its geographical, economic and sociocultural factors. Infrastructure as basic as electricity is still not distributed evenly, where eastern provinces, such as Nusa Tenggara and eastern Papua, only have an electrification ratio of 60%.27,28 Poor infrastructure in transportation, communication networks and healthcare are exacerbated by the fact that Indonesia is one of the largest archipelago nations. In terms of information systems, one big challenge that Indonesia needs to overcome is interoperability, which refers to the capacity of health information systems to collaborate seamlessly within and across organisational borders.29 Without interoperability, the development of new digital-based cardiac prevention devices or applications will only create scattered and fragmented data across multiple platforms. For digital cardiac prevention to be successful, these barriers should be addressed simultaneously with the creation of new regulation regarding telehealth and mhealth to ensure the legality of these new technologies and equal distribution of their services, while maintaining the protection of patients’ data and confidentiality.
Research on digital health in Indonesia has been conducted in various health system domains. However, when focusing on cardiovascular prevention and rehabilitation care, available studies are limited and in the form of small pilot studies. One of the more prominent mhealth initiatives for CVD primary prevention is SMARThealth (Systematic Medical Appraisal Referral and Treatment), a multifaceted primary healthcare intervention supported by mobile technology. Its objective is to enhance the delivery of guideline-based assessment and management of CVD risks.
A quasi-experimental study was conducted on 6,579 CVD high-risk individuals in eight rural villages in the Malang district, and yielded increased usage of preventive CVD medication and lower blood pressure levels after participating in the programme.30 In contrast, to our knowledge, no digital innovation for CVD secondary prevention has ever been developed in Indonesia. CR should have an integral part when incorporating digital healthcare into CVD management. In this regard, the opportunity arises for future Indonesian innovators and researchers to develop a new digital-based approach for CR, and validating it through clinical trials.
Future direction for digital cardiac prevention in Indonesia has been directed by the Ministry of Health with the release of the Blueprint for Digital Health Transformation Strategy 2024. It focuses on finding the solution for millions of health data fragmentation caused by the ≥400 health applications developed by local and central government, which are not integrated to one another; thus, underutilising the benefit of those applications. With three key activities of integrating and developing health data, an application system, and technology ecosystem, it is expected to help improve health policy, increase efficiency of health services and create collaboration in digital health ecosystem involving stakeholders. This means that in the future, any innovation in the field of cardiac prevention could benefit from a singular electronic medical record by using an integrated healthcare system platform.12
With the rise of natural-language processing AI, such as ChatGPT, Gemini and Bing, new opportunities for using this tool in assessing and managing risk factors of cardiac prevention have opened.31,32 Using natural-language processing AI, patients can potentially interact with a chat-based interface, and it is becoming an increasingly popular model for an AI-based cardiac prevention programme.33,34 However, developing natural language processing AI for cardiac prevention in Indonesia is not without its challenges. For instance, designing this type of AI requires consideration of the AI’s ability to personalise and contextualise information for Indonesia’s hugely diverse ethnic and language groups. Additionally, infrastructures, such as high computing-power hardware, and a centralised and standardised health data, are also important to the development of AI.35
Despite the challenges, the Indonesian government is committed in establishing an AI-driven health data analysis system contingent on the completion of the nationwide Integrated Electronic Medical and Health Record, as outlined in the 2024 Blueprint for Digital Health Transformation Strategy.12
Factors for a Successful Programme
Although an increasing number of pilot telemedicine projects for cardiac prevention have been conducted, only a few have been embedded in everyday practice in clinical and healthcare settings. Many projects are discontinued at the end of their pilot studies. With poorly coordinated initiatives, a lack of investment and inadequate usage of the telemedicine service on a comprehensive network, it becomes doubtful how beneficial this technology solution can be for all parties involved, which consequently results in poor service delivery. Therefore, many questions need to be addressed before a sustainable programme can be strategically deployed on a large scale across the different regions of a country (Figure 1).
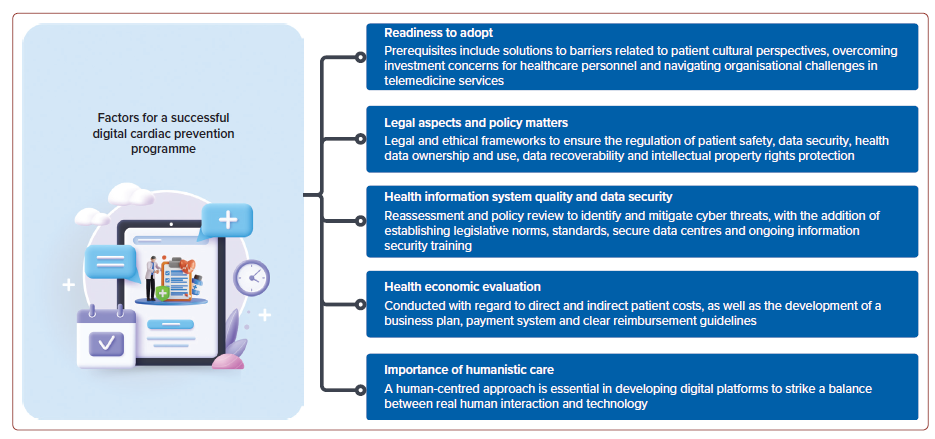
Readiness to Adopt
The development of digital healthcare has primarily been driven by technology, often without sufficient consideration for the perspectives and needs of the individuals they are intended to benefit. To effectively implement a system for digital-based cardiovascular prevention on a broader scale, it is essential to address the crucial roles, needs, and expectations of both cardiovascular patients and physicians.
Patient-oriented Barriers and Proposed Solutions
The adoption of telemedicine varies among different populations, influenced by factors, such as patient characteristics, digital literacy and health literacy. Older age, low health literacy, and lower socio-economic and health status have been linked to reduced usage of digital health services. Unfortunately, these are the very groups that cardiovascular prevention efforts often target. Age significantly shapes health information-seeking behaviour, with individuals of lower educational attainment less likely to seek health information online or use websites for health-related tracking.36 Limited health literacy is often associated with low socio-economic status, as seen in the European Health Literacy survey.37 Additionally, some individuals perceive limited value in digital health services, preferring in-person doctor visits for a more personalised experience, considering digital healthcare as an adjunct option.7
Incorporating digital technology into traditional care can facilitate the gradual transition of patients into the digital ecosystem, empowering them to take a central role in managing their own diseases, while allowing physicians to refine their treatment choices. Further research should focus on specific populations, such as those of low socio-economic status, low digital literacy or the elderly, to evaluate the impact and risks of social inequalities, and develop strategies to address them.
Physician-oriented Barriers and Proposed Solutions
While wireless technologies enable daily monitoring of cardiovascular risks, healthcare personnel may perceive a significant investment is required to initiate such programmes. These personnel play a crucial role in facilitating the transition to the digital ecosystem, and bridging the gap between patients and technology communities. They are expected to invest time and effort in reviewing and providing feedback on incoming data, seeking feedback on digital services and optimising the system. Meanwhile, physicians have existing responsibilities attending to hospitalbased appointments and administrative tasks.7
In Indonesia, concerns regarding the overall wellbeing of healthcare workers raise questions about the readiness of the digital healthcare system to be implemented on a broader scale, particularly considering the already heavy workload of these workers. Physicians and other healthcare professionals receive relatively low remuneration, which is disproportionate to the services they provide and the long working hours they endure, with junior doctors earning approximately $250 monthly.38 The Indonesian Medical Association has a responsibility to advocate for the rights and concerns of physicians, including income distribution policies, ensuring a safe working environment, and fostering public trust and respect, as these factors influence physicians’ welfare, wellness and job satisfaction.39 Addressing mental and physical burnout is crucial to maintaining physicians’ performance in delivering quality healthcare.40
Healthcare System-related Barriers and Proposed Solutions
Previous models of digital healthcare, such as the United4Health project in Europe, enabled remote monitoring of patients with chronic diseases, fostering their self-management under physician oversight. Although not a randomised controlled trial, the project was supported by RENEWING Health, a larger study demonstrating positive clinical outcomes and staff satisfaction. Patient-friendly and affordable telehealth systems hold appeal for patients and their families.41 However, despite implementing similar telemedicine protocols and interventions across different sites in the United4Health project, organisational set-ups varied widely. The development of a universal model remains elusive, with healthcare organisational structures posing significant challenges for telemedicine services.42 Addressing organisational aspects, as proposed by the Pan American Health Organization and WHO, including process, structure, financing, management and cultural considerations between organisations, can reduce cooperation barriers and facilitate knowledge transfer.43
Successful implementation of telemedicine services necessitates the creation of clear standard operating procedures, a defined chain of command, explicit expectations and objectives, and the allocation of functions and responsibilities from the outset. Additionally, health policy objectives related to security, ethics, legal requirements and data protection must be established. Involvement of healthcare professionals in decision-making processes, and the presence of a robust business plan to secure funding and resources are crucial. Furthermore, effective governance mechanisms and continuous evaluation methods should be implemented to ensure the sustainability of the programme.43
Finally, cultural factors play a significant role and must be carefully considered. Some individuals, particularly those of older generations, may exhibit hesitancy in adopting new technologies or processes due to initial uncertainties. In many Asian countries, where workplace culture is deeply rooted in seniority and individual performance-based systems, Western approaches often do not align well.44 Both systems have their merits, but aligning all participants towards the use of new digital technologies in healthcare requires substantial effort and strategic considerations.
Legal Aspects and Policy Matters
Successful change in cardiac prevention digital health necessitates both bottom-up willingness and top-down policy support. A comprehensive telemedicine policy initiative is required to expedite and harmonise the deployment of a framework that aligns with evolving health policies, systems and practices. The establishment of regulations on reimbursement incentives is crucial to support the future integration of digital healthcare services. Furthermore, new service delivery models should prioritise evidence-based clinical practice, and carefully consider the availability, interoperability, and maturity of the information and communication technology infrastructure in each country. Safety concerns related to remote management in the medical context, as well as legal implications regarding clinical supervisors’ responsibility for monitoring device data, must also be addressed within the unique regulatory and healthcare landscapes of each country.41
Regarding legal and policy considerations, the WHO recommends the adoption of legal and ethical frameworks to ensure adequate regulation of patient safety, data security, health data ownership and use, privacy, data recoverability, and intellectual property rights protection.43 Even countries with advanced e-governance and cybersecurity face challenges in safeguarding patient privacy, as cyber threats can have significant socio-economic consequences. In Europe, the General Data Protection Regulation addresses data protection and privacy for EU citizens, including the transfer of personal data outside the EU, aiming to empower individuals and establish overarching regulations for international businesses.15
Indonesia already has detailed legislation on personal data protection through the Regulation of the Minister of Communication and Informatics of the Republic of Indonesia No. 20 of 2016, specifically addressing personal data protection in electronic systems.45 Strengthening privacy and security measures, legislation amendments should encompass medical software, including cardiovascular mhealth apps and medical devices, and mandate quality control through regular validation and verification based on state-of-the-art standards.
Health Information System Quality and Data Security
To ensure the secure handling of patients’ medical information, comprehensive measures are needed. Legislative norms and standards should be established to define requirements, rights, and obligations regarding access and use of personal medical data. All databases and information systems should be managed in secure data centres that meet national information security standards. Ongoing training on information security is essential.
The level of accessibility for visualisation, analysis and integration of acquired data into electronic health records for clinical use is a topic of debate. Interoperability enables information sharing among applications without compromising data content and quality, ensuring continuity of care across various patient contexts and caregivers.
Some countries, such as Estonia and Dubai, have effectively implemented blockchain technology for the security and transparency of patients’ medical records. Rather than storing data in a single database, blockchain allows multiple synchronised copies to be shared across a network of users. This enables reliable access to patient data for doctors, pharmacists and other medical professionals. Such a system enhances care in acute, life-threatening situations and chronic disease management. With strict privacy limitations, the data can also be shared with insurers or state agencies to facilitate efficient transactions across governmental and private entities. Patients are the primary beneficiaries, as they can accurately view their medical data in real time. Any changes to the record by state agencies, private organisations or malicious hackers would be visible to the entire network, including the patient. This concept of individual empowerment and medical transparency has revolutionary potential. Considering such forward-thinking technology would be valuable for the future advancement of the Indonesian healthcare system.
The Indonesian government’s cyber defence policy, in Presidential Regulation No. 97 of 2015, lacks comprehensive elaboration on national cyber defence. To enhance this policy, the government should reassess potential cyber threats to national security. The current definition of ‘national vital object’ is limited to tangible assets, whereas the US and the European Union have broader definitions that include virtual systems and assets. A policy review of Presidential Decree No. 63 of 2004 is necessary to identify vital sectors in Indonesia, such as national health services, susceptible to cyberattacks, and formulate appropriate defence and mitigation strategies.46
Health Economic Evaluation
Conducting economic evaluations of digital-based cardiovascular healthcare is crucial to inform health insurance industries about the value for money and support decision-making. It is important to develop a business plan and payment system for large-scale deployment of digital health services. Patients should have the ability to claim healthcare services facilitated by digital technology through insurance plans, while clinicians should be appropriately reimbursed for their services. Clear guidelines, policies and procedures should be implemented in relation to reimbursement for digital health services.
Currently, there is a lack of reimbursement models for these services. However, reimbursement should consider direct and indirect patient costs, intervention costs (from suppliers to healthcare clinics and specialists), as well as start-up investments required for establishing new healthcare strategies. Direct patient costs encompass initial cardiac hospitalisation and rehabilitation, while indirect patient costs include productivity loss due to premature mortality or rehospitalisation.
Several studies have investigated the cost-effectiveness of digital healthcare programmes. While one study suggested that telerehabilitation may not be cost-effective due to higher intervention costs compared with the gain in quality-adjusted life years, other studies have shown that cardiac secondary prevention strategies through digital care are more cost-effective than traditional cardiac rehabilitation. These studies have also demonstrated a reduction in cardiovascular rehospitalisations and days lost.47-49 While micro-economically digital health interventions can be cost-saving for individual patients in the long term, there may be a net rise in healthcare expenditure due to increased demand. Cost–utility analysis can help compare costs and health effects of alternative interventions, and guide resource allocation decisions in different healthcare settings.50
Will it Replace Humanistic Care?
Undoubtedly, digital technology plays a vital role in healthcare services and is considered essential for future success. However, there are limitations to its application in the medical field. It cannot fully replace human qualities, such as creativity, intuition and experience, which are unique to healthcare providers. As social beings, humans require genuine interactions that cannot be replicated by technology relying solely on instructions and algorithms. Therefore, in the development of digital platforms, the element of service delivery must maintain a human-centred approach. It is crucial to strike a balance between real human interaction and services offered through digital platforms by integrating the two. Technology should aim to enhance the quality and quantity of the clinician–patient relationship, particularly for patients with chronic conditions or limited resources for frequent visits to the doctor’s office. Sensors, smartphone apps, monitoring devices and telerehabilitation programmes should facilitate active engagement from both patients and physicians. Algorithms can be developed to alert healthcare providers when a situation requires their immediate attention, enabling targeted care where a human touch is necessary.
Conclusion
The undeniable role of digital technology in the advancement of CVD prevention becomes even more crucial in the face of challenges, such as COVID-19, with lockdowns and social distancing mandates highlighting the need for accessible cardiovascular prevention and rehabilitation in remote areas. Start-ups and technology giants are actively pursuing opportunities in the digital health sector, while governments across various socio-economic levels are beginning to allocate funding and resources to support this transformation. However, the regulatory framework in this field is still inadequate. Numerous obstacles must be addressed, including user readiness, legal and policy considerations, health information system quality, data privacy and protection, cost–benefit analysis, and the potential loss of essential human interaction.
Learning from countries that have significant experience in the digital healthcare industry will undoubtedly be beneficial. As we embrace and integrate these technologies into the development and implementation of digital cardiovascular prevention programs, it is crucial to recognise that each country has its unique healthcare system, culture and beliefs upheld by its citizens. Every effort should be made with the ultimate goal of improving outcomes for all parties involved.
Clinical Perspective
- This review is the first to assess the current condition of digital healthcare for cardiac prevention programmes in Indonesia
- It is crucial to analyse the experiences of other prominent nations, as they offer valuable insights that can guide Indonesia in advancing its digital healthcare initiatives for cardiac prevention.
- Additionally, this review outlines key factors essential for the successful implementation of digital healthcare for cardiac prevention with consideration to Indonesia’s specific circumstances.