Since the outbreak of the severe acute respiratory syndrome coronavirus 2 pandemic in 2019, COVID-19 has spread across the globe, resulting in millions of deaths worldwide. Beyond an immediate impact on mortality and morbidity, this pandemic has also had secondary ramifications for the provision of healthcare as hospitals change existing workflows to accommodate the screening and treatment of COVID and governments impose lockdown measures that directly and indirectly affect patients’ presentation to hospitals.
Studies have been published about the effect of the COVID-19 pandemic on procedural volumes of elective percutaneous coronary intervention (PCI), as well as on the presentations and outcomes of acute MI (AMI).1–5 Many of these studies only capture the perspective of a single centre in a particular country. Furthermore, study findings are mixed, with some studies reporting a decrease in non-ST segment elevation MI (NSTEMI) or ST-elevation MI (STEMI) presentations since the onset of the pandemic, and others finding no significant difference, particularly in the STEMI caseload.1–5 Similarly, reported effects on door-to-balloon (DTB) time and mortality outcomes are mixed.1
The aim of this study was to investigate the effects of the COVID-19 pandemic on AMI and PCI rates in countries from Asia and the Middle East to gain an insight into the burden COVID-19 was placing on cardiovascular care. This research is especially pertinent because many of these countries are facing repeated waves of COVID-19, and lessons drawn from earlier experiences will be instructive in preparing for future outbreaks.
Methods
Member countries from the Asian Pacific Society of Cardiology were invited to submit pooled data on cases with discharge diagnoses of AMI or PCI, as defined by prespecified ICD codes. Records for admissions for AMI were further subdivided into diagnoses of NSTEMI and STEMI. In-hospital case fatality data were collected for each of these admissions.
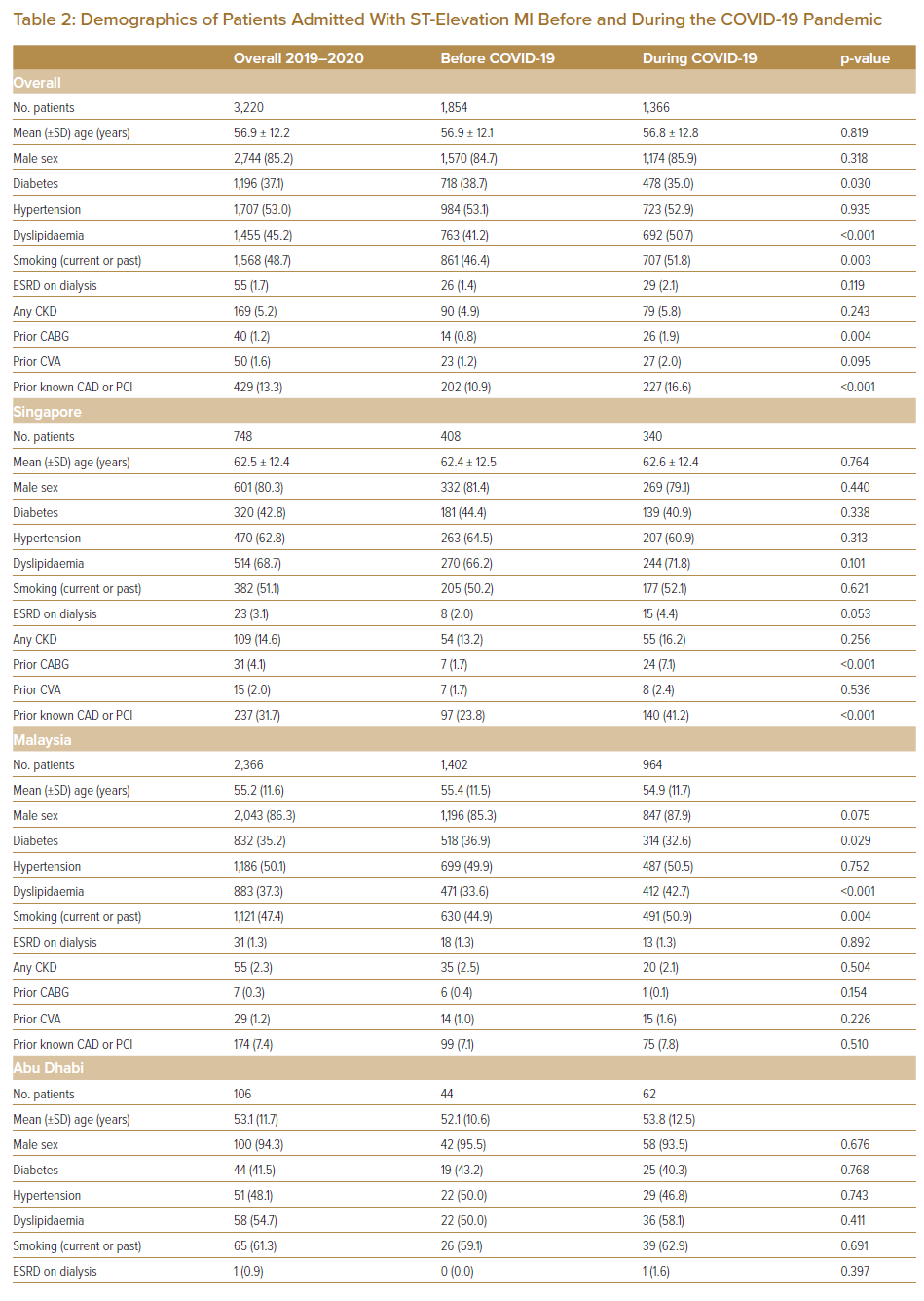
In addition, data on patient demographics, comorbidities and DTB time were collected for STEMI admissions. We chose STEMI cases for closer analysis because STEMI is a well-defined clinical entity, with established guidelines around the diagnosis and management of the condition, thus making it a good substrate for comparison of patient profiles before and during the COVID-19 pandemic.
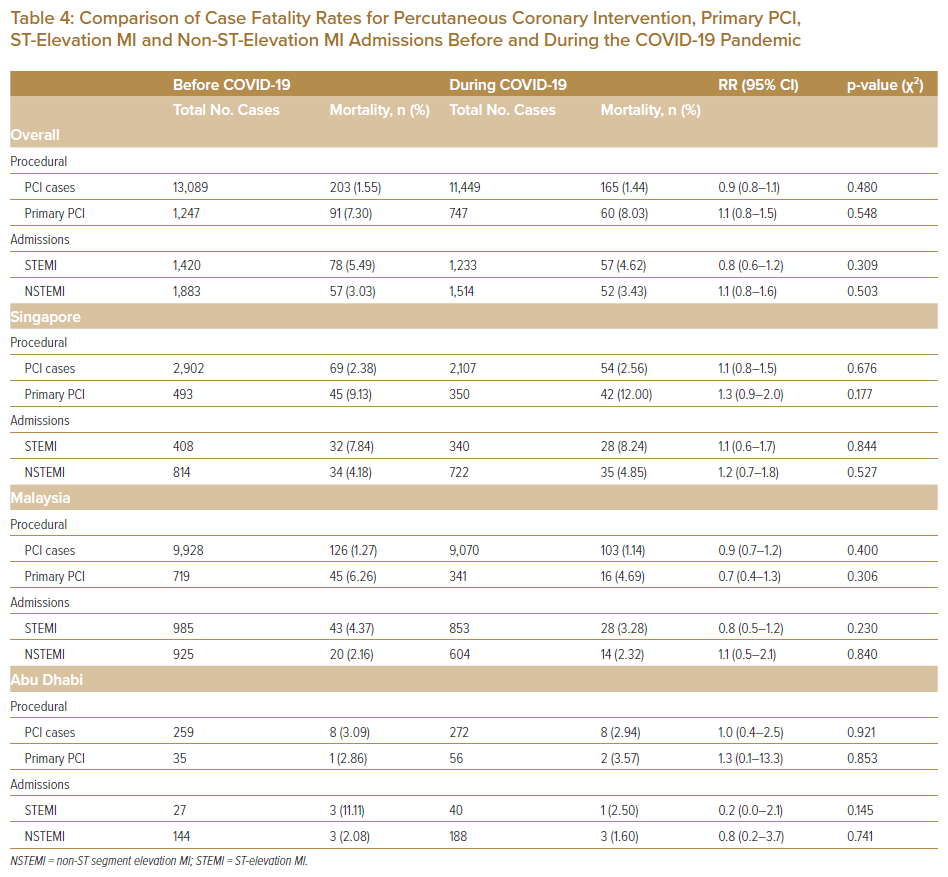
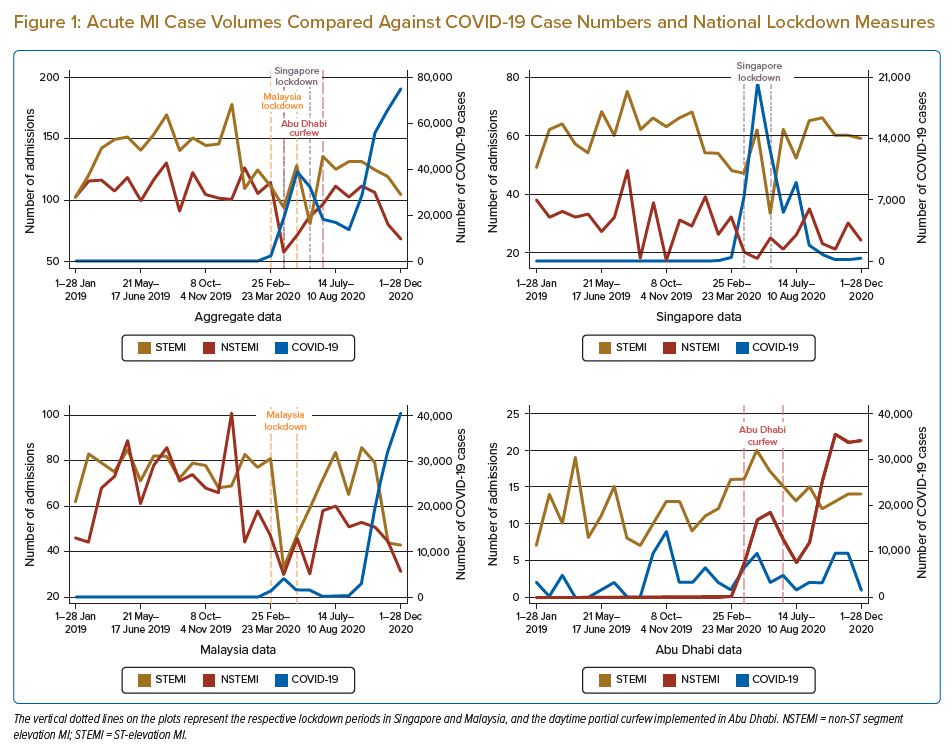
Three centres responded to the call for data: the National Heart Association of Malaysia, which indexes all PCI and AMI data in Malaysia; the National Heart Centre Singapore, a tertiary hospital with the highest PCI case volume in Singapore; and the Cleveland Clinic Abu Dhabi, a private tertiary hospital in Abu Dhabi. AMI and PCI case volumes were reported in 4-weekly blocks and plotted against COVID-19 case numbers in each respective country for the corresponding time block (Figures 1 and 2).
Statistical Analysis
Statistical significance was set at two-tailed p<0.05. Continuous variables are presented as the median with interquartile range (IQR) and categorical variables are presented as frequencies and percentages. Comparisons between the pre- and during COVID-19 periods were made using χ-squared or Fisher exact tests, as appropriate, for categorical variables and two-sample t-tests or the Kruskal–Wallis test for continuous variables. The relative risk of mortality was calculated based on 2 × 2 contingency tables. Percentage changes were calculated by comparing the admissions and procedural volumes of the respective 4-week blocks for 2019 with the same period in 2020.
All statistical analyses were conducted using Stata version 16 (StataCorp).
Results
Acute MI
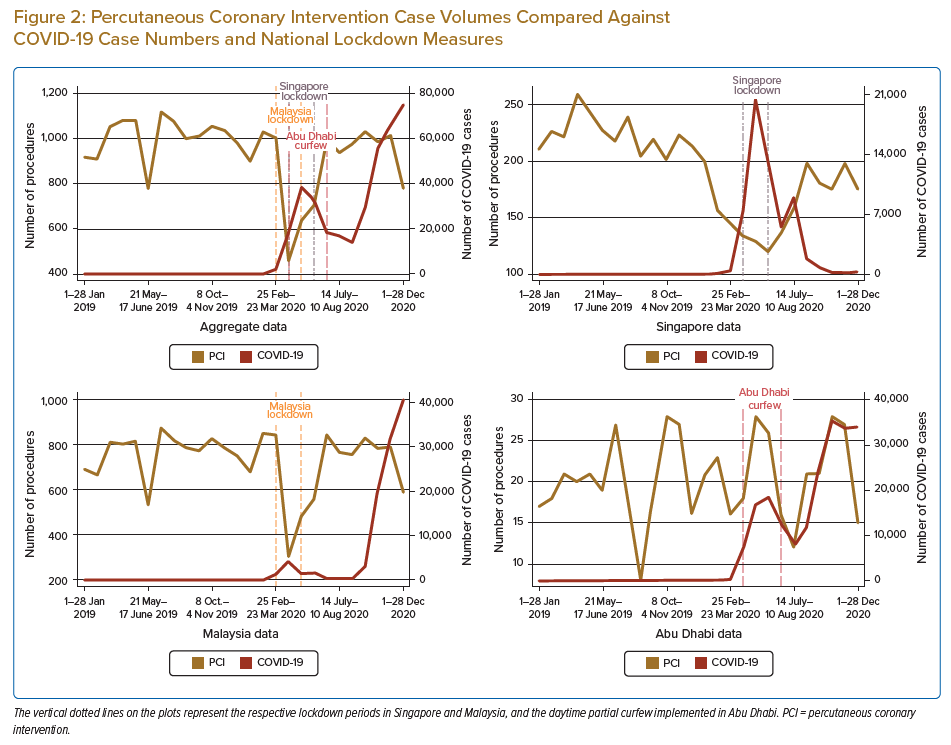
Overall, 3,661 patients were admitted for AMI during the pre-COVID-19 period, compared with 2,968 during the COVID-19 period (p<0.001). Although there was no difference in the number of STEMI admissions before and during the COVID-19 period (1,420 versus 1,233; p=0.081), there was a significant reduction in NSTEMI admissions (1,883 versus 1,514; p<0.001; Tables 1 and 2).
Looking at data from individual countries, both Singapore and Malaysia experienced a reduction in total AMI admissions, driven primarily by a reduction in NSTEMI presentations. In Singapore, NSTEMI cases fell from 814 before the pandemic to 722 during the pandemic (p=0.025). Similarly, in Malaysia, NSTEMI cases fell from 925 before the pandemic to 604 during the pandemic (p<0.001). However, in Abu Dhabi, there was a significant increase in NSTEMI cases (144 to 188; p=0.010). There was no significant difference in STEMI cases from before to during the pandemic in any of the three countries.
Patients admitted with STEMI during the COVID-19 period, compared with those admitted prior to the pandemic, were less likely to have diabetes (35.0% versus 38.7%; p=0.030), more likely to have dyslipidaemia (50.7% versus 41.2%; p<0.001), more likely to have had prior coronary artery bypass grafting (1.9% versus 0.8%; p=0.004) and more likely to have had prior coronary artery disease or PCI (16.6% versus 10.9%; p<0.001). Overall, there was a significant decrease in the proportion of cases achieving a DTB time of ≤90 minutes during the COVID-19 period (59.89% versus 76.81%; p<0.001 (Table 3).
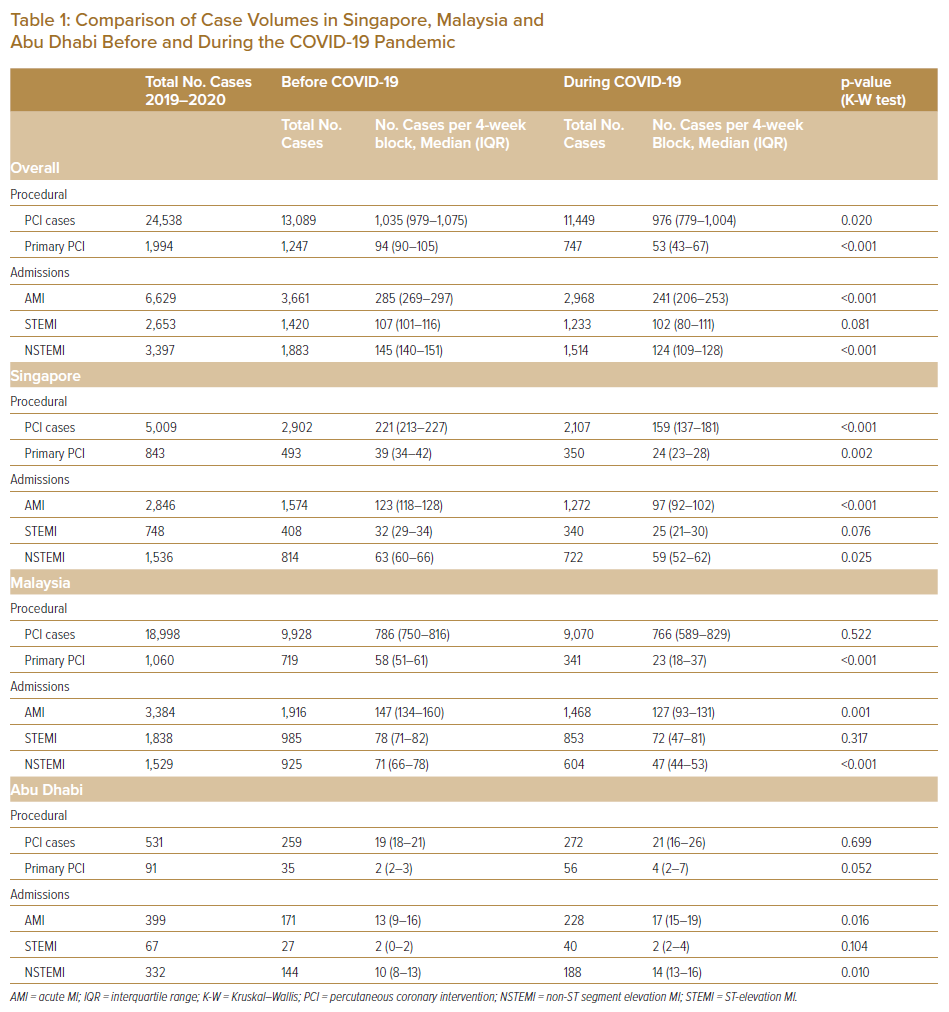
In Malaysia, there was a significant reduction in proportion of cases with a DTB time ≤90 minutes during the pandemic (39.00% versus 71.21%; p<0.001). However, there was no difference in the proportion of cases with a DTB time ≤90 minutes in Singapore and Abu Dhabi with >95% of cases having a DTB ≤90 minutes in both countries. There was no significant difference before and during COVID-19 in in-hospital mortality for STEMI patients (5.49% versus 4.62%; p=0.309) or in in-hospital mortality for NSTEMI patients (3.03% versus 3.43%; p=0.503). Similarly, individual country analysis did not yield any significant differences in case fatality rates for STEMI or NSTEMI patients before and during COVID-19 (Table 4).
PCI Volume
Overall, there was a significant decrease in PCI cases from before to during the COVID-19 period (13,089 versus 11,449; p=0.020). This was driven mostly by data from Singapore, where the number of PCI cases decreased from 2,902 before the pandemic to 2,107 during the pandemic (p<0.001). In contrast, the PCI caseload in Malaysia and Abu Dhabi remained relatively constant (p>0.05). Overall, there was no significant difference in the case fatality rate from before to during the COVID-19 pandemic (1.55% versus 1.44%, respectively; p=0.480).
Discussion
Data pertaining to the impact of COVID-19 on cases of AMI are varied. Several centres have reported a decrease in admissions during the pandemic,1,2,6 whereas others have found no significant difference compared with pre-COVID-19 levels.5 With regard to the type of MI, most studies have shown a decrease in NSTEMI admissions during the COVID-19 pandemic, but mixed results pertaining to STEMI presentations.3,7
Similarly, in the present study there was a decrease in NSTEMI admissions, but we did not find any significant difference in STEMI presentations between the two periods. It is conceivable that STEMI patients experience more severe symptoms that will push them to seek medical attention. Furthermore, they will also have distinct ECG abnormalities that prompt urgent referral to tertiary centres by primary care or emergency medical services. This stands in contrast to the symptoms in NSTEMI, which may be less typical and less intense, such that they are tolerated by patients, who refrain from presenting to hospital for fear of being exposed to COVID-19.
There is high health avoidance behaviour during pandemics, especially when there are unconfirmed beliefs about modes of transmission, increased perceived severity of the outbreak and increased perception of susceptibility.8,9 Indeed, nadir levels of NSTEMI and STEMI admissions in Malaysia and Singapore were reached during the respective lockdown periods in each country. In particular, NSTEMI and STEMI admissions in Malaysia were lowest during the period 24 March–20 April 2020, which coincided with the start of the Movement Control Order (18 March–3 May 2020). This is despite the fact that the absolute number of COVID-19 cases was higher in the latter part of 2020. This suggests that fear surrounding the initial outbreak of a hitherto unknown virus, along with the added psychological burden of a government-imposed curfew, may have been holding patients back from presenting to hospital, despite the fact that they were still allowed to seek medical attention during these lockdown periods.
NSTEMI and STEMI admissions in Abu Dhabi rose in tandem with the number of COVID-19 cases in the country, which is in contrast to data from Singapore and Malaysia. This reflects the impact of local policy, because the Cleveland Clinic Abu Dhabi was designated by the public health authorities as a centre responsible for care of non-COVID-19 conditions. This resulted in NSTEMI and STEMI cases being diverted to this centre.
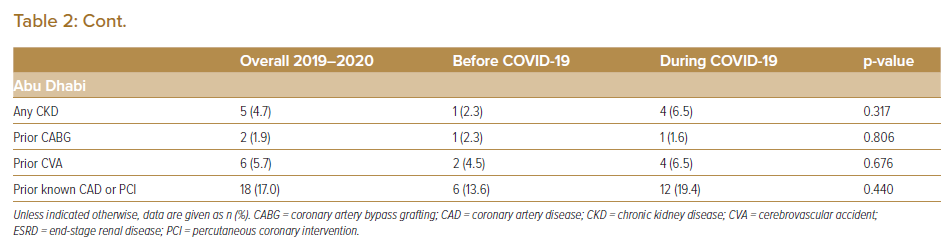
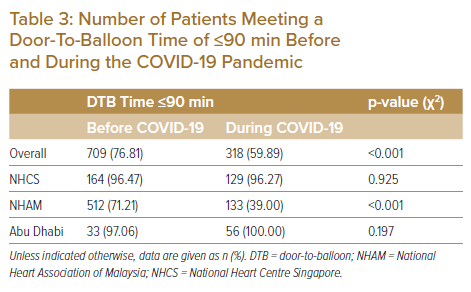
In this study, the proportion of patients achieving a DTB of ≤90 minutes was reduced in Malaysia, but unchanged in Singapore and Abu Dhabi. Notably, of the three countries, Malaysia pursued a thrombolysis-first strategy, with primary PCI only if the patient was known to be COVID-19-negative or as rescue therapy in the event of failed thrombolysis with medical staff in full personal protective equipment.10 This would likely explain the difference in DTB time among the three countries. Other studies with similar findings have attributed differences in DTB time to the time taken to perform preadmission screening chest X-rays and to ascertain travel and contact histories and symptomatology in patients whose COVID-19 status is unknown.1,11 Unfamiliarity of the emergency department (ED) with new workflows may also be a contributing factor, with subsequent recovery in the DTB time towards the later stages of the pandemic.12 Data from Singapore and Abu Dhabi suggest that with appropriate and well-rehearsed ED workflows, a strategy of primary PCI can still be pursued for STEMI care, with little effect on overall DTB time. This is especially important in a prolonged pandemic response, given the superior outcomes of a primary PCI strategy.13
Nevertheless, despite the increase in DTB time, we did not find a corresponding significant increase in STEMI in-hospital mortality. Similarly, case fatality rates for NSTEMI, PCI and primary PCI remained largely constant. This is in keeping with reports from other studies, and is testament to the robustness of these medical systems in maintaining a high level of cardiovascular care despite the pandemic.1,6,14
Data on PCI volumes provide some insights into how COVID-19 has affected elective procedures. The decrease in PCI in the present study was driven largely by data from Singapore, where there was an active push to reschedule non-urgent elective cardiac catheterisation. The decline in PCI in Singapore started with the onset of the COVID-19 pandemic and reached a nadir during the government-imposed ‘circuit breaker’ (7 April–1 June 2020). The fall can be explained by guidance from the Ministry of Health in Singapore and individual institutions to postpone non-urgent cases to free up bed space in anticipation of a surge in COVID-19-related admissions. Recovery ensued as healthcare systems adapted.
Limitations
Although this study sheds light on the effect of COVID-19 on cardiovascular care in Singapore, Malaysia and Abu Dhabi, the insights are largely limited to these countries and constrained by the particular circumstances of each country’s response to COVID-19. In addition, the data from Singapore and Abu Dhabi are from a single centre and may not be fully generalisable. As we highlighted earlier, reports on the effects of COVID-19 are context dependent and can differ greatly. Furthermore, our study concluded in December 2020, when case numbers in Malaysia and Abu Dhabi were still increasing. Further research into the effects of these second waves will be very instructive in ascertaining how healthcare systems deal with far higher COVID-19 case numbers despite being armed with protocols and experience in operating under pandemic conditions.
Conclusion
This study has shown that the COVID-19 pandemic has led to a fall in NSTEMI, but not STEMI, admissions. A reduction in the proportion of STEMI patients achieving a DTB time of ≤90 minutes may be related to the thrombolysis-first approach pursued by Malaysia. PCI volumes decreased, primarily driven by the deferral of non-urgent procedures in Singapore. There was no significant effect of the COVID-19 pandemic on in-hospital mortality.
Clinical Perspective
- The COVID-19 pandemic resulted in a fall in non-ST segment elevation MI but not ST-elevation MI (STEMI) admissions in Singapore and Malaysia. This decrease appears to be related more to the implementation of nationwide lockdown measures rather than absolute COVID-19 case numbers.
- A reduction in the proportion of STEMI patients achieving a door-to-balloon time of ≤90 min may be related to the thrombolysis-first approach pursued by Malaysia.
- PCI volumes decreased due to deferral of non-urgent procedures, especially in Singapore.
- There was no significant effect of the COVID-19 pandemic on case fatalities from acute MI admissions or percutaneous coronary intervention procedures.