A critical challenge in the management of patients with heart failure with reduced ejection fraction (HFrEF) includes suboptimal use and dose uptitration of prognostically significant guideline-directed medical therapy (GDMT), as demonstrated in various registries, such as ASIAN-HF and CHAMP-HF.1,2 It is likely that failure to achieve recommended dosing is partly attributable to the length of time required to uptitrate to maximum dose, with patients less likely to adhere to multiple medications and lengthy treatment processes. Combination pills, or polypills, have been proposed previously to tackle such clinical inertia, due to how the strategy has been employed successfully in many other conditions, including malaria, tuberculosis and hypertension.3 However, little is known regarding perceptions surrounding rapid initiation and uptitration, currently advocated by many leaders in the heart failure field following positive results from the recent STRONG-HF trial.4 Furthermore, far less is known about the perceptions of a polypill strategy in managing heart failure. This study aimed to assess readiness among cardiologists and cardiology fellows-in-training (FIT) in using a polypill strategy in the management of HFrEF.
A national-level, 21-item survey study was conducted between 1 January 2023 and 30 June 2023. The survey was administered electronically via Google Forms. Participants were invited via email communication through the National Heart Association of Malaysia’s weekly newsletter. Participants consisted of cardiology FIT, post-fellowship cardiologists and consultant cardiologists. Clinical information was obtained from participants, and included demographic characteristics, current approaches, and challenges in managing HFrEF, as well as knowledge, attitudes and perception surrounding using a polypill strategy in the management of HFrEF. Ethical approval was granted for the study (REC/12/2021 [MR/976]). Results are expressed as mean and standard deviation for continuous variables, or as number of cases and percentages for categorical variables.
A total of 120 participants responded to the survey, of which 53.3% identified as male (Table 1). Up to two-thirds had more than a decade of clinical experience, with an equal split in response from both cardiology FIT and those who were post training. There was also an equal split in response seen between participants who, in their current practice, initiate GDMT in a stepwise manner, versus those who prescribe various GDMT simultaneously.
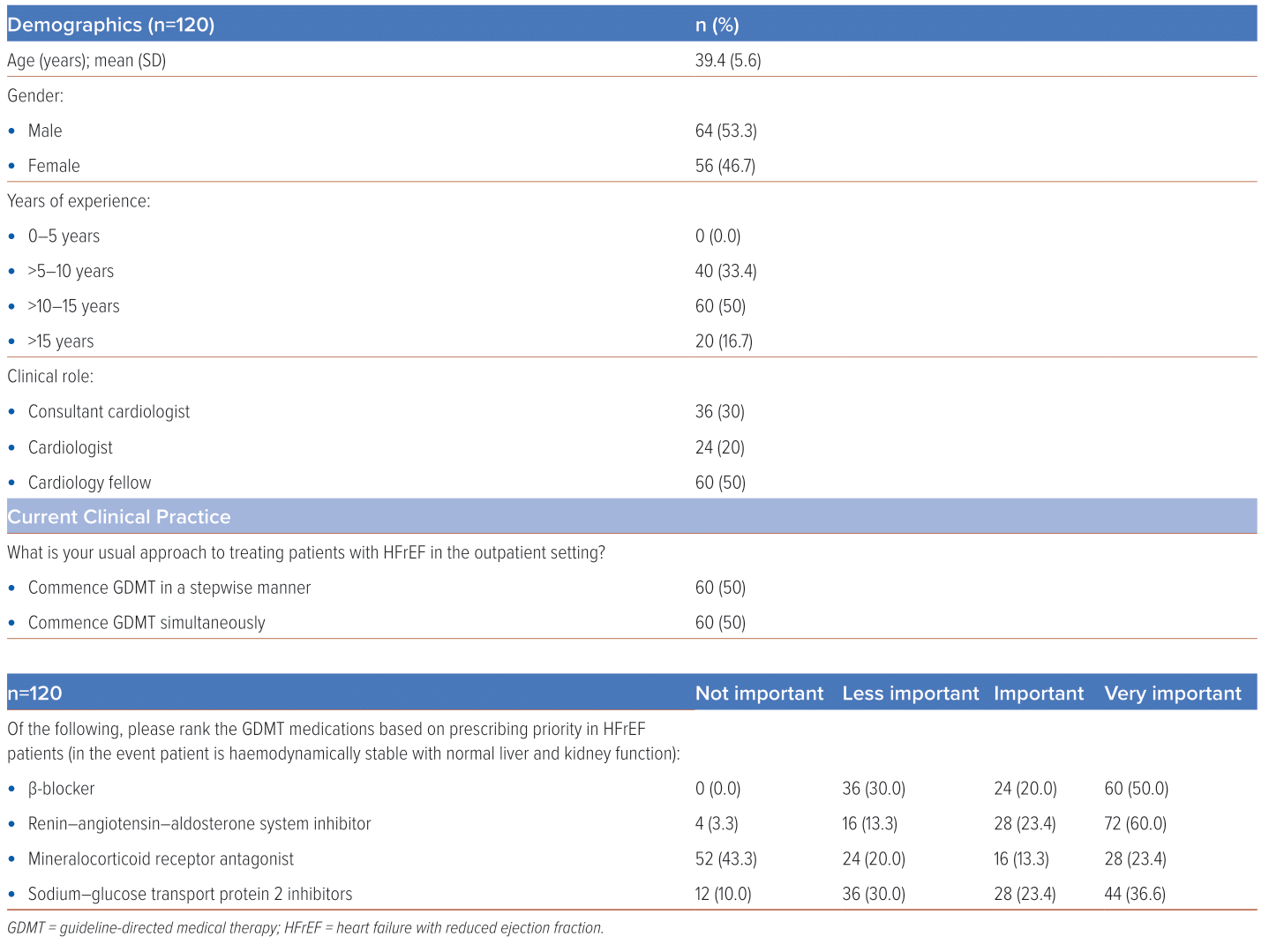
A large proportion of participants believe that both β-blockade (BB) and renin–angiotensin–aldosterone system inhibition (RAASI) were “important” or “very important” (70.0–83.4%), unlike mineralocorticoid antagonist (MRA). This likely reflects attitudes that mimic traditional, sequential initiation of GDMT in older guidelines.5 Surprisingly, the proportion of respondents who felt that sodium–glucose transport protein 2 inhibitors (SGLT2Is) were “important” or “very important” was far higher than MRA, likely due to heightened attention surrounding this drug class over the past decade.
Potential challenges that may occur when prescribing a polypill in managing patients with HFrEF included challenging haemodynamic (76.7%), anxiety surrounding kidney function deterioration (70.0%), and both costs and reimbursement (50.0%; Table 2). Nevertheless, the majority felt that a polypill approach remained ethical, despite the potential adverse effects and lack of trial-based evidence in adopting a polypill strategy therapy for heart failure. A higher proportion of respondents would consider swapping to a polypill strategy only after appropriate dosing of each individual GDMT component (56.7%), and that polypills should exist with various dosing combinations (90.0%). Of those respondents currently adopting a stepwise approach in GDMT prescription, 3.3% did not believe in a polypill strategy. Interestingly, of these respondents, 30.0% would consider a polypill for their patients once they have uptitrated all GDMT maximally, and 16.7% were open to immediately swapping their patients over to a polypill if available.
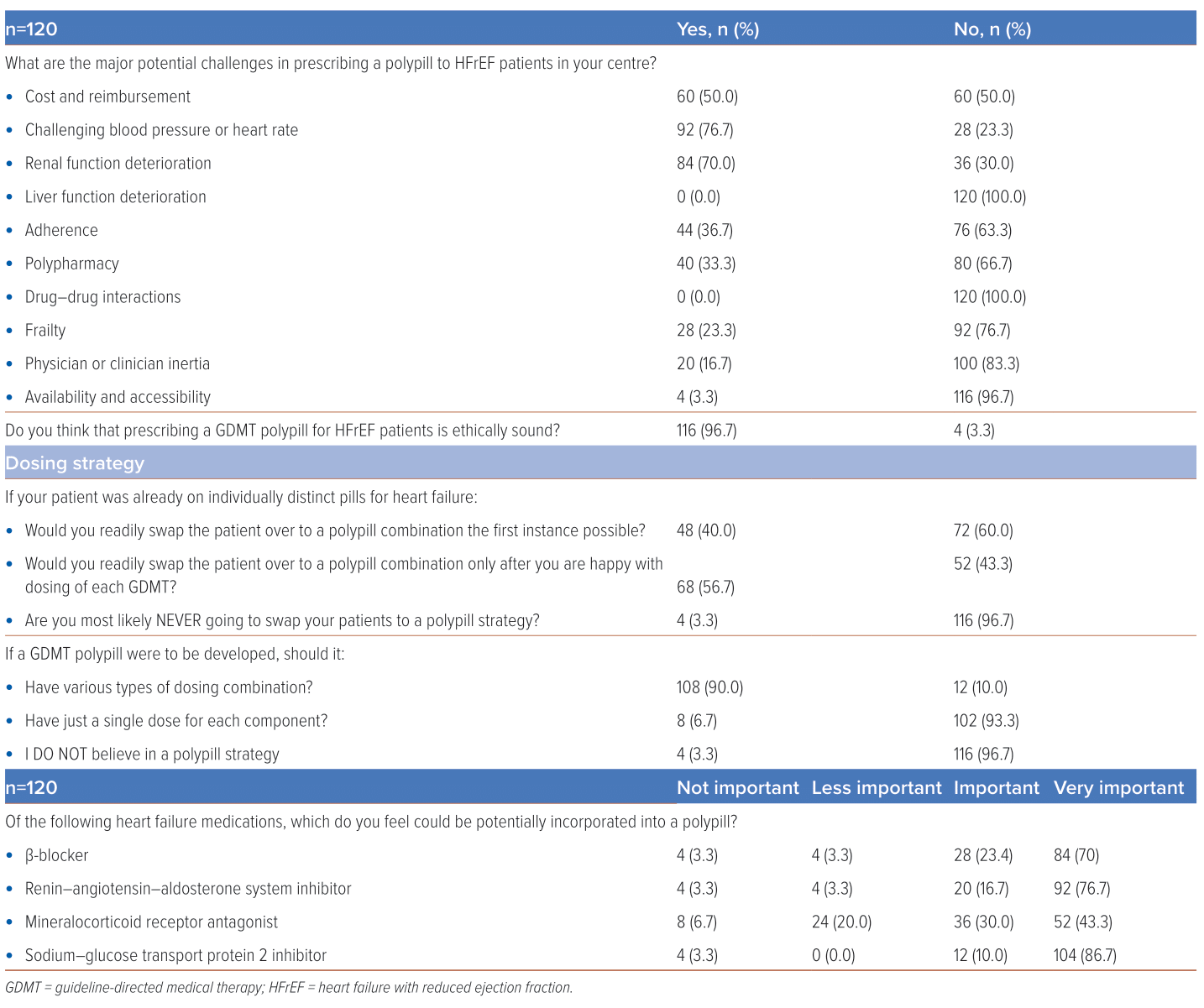
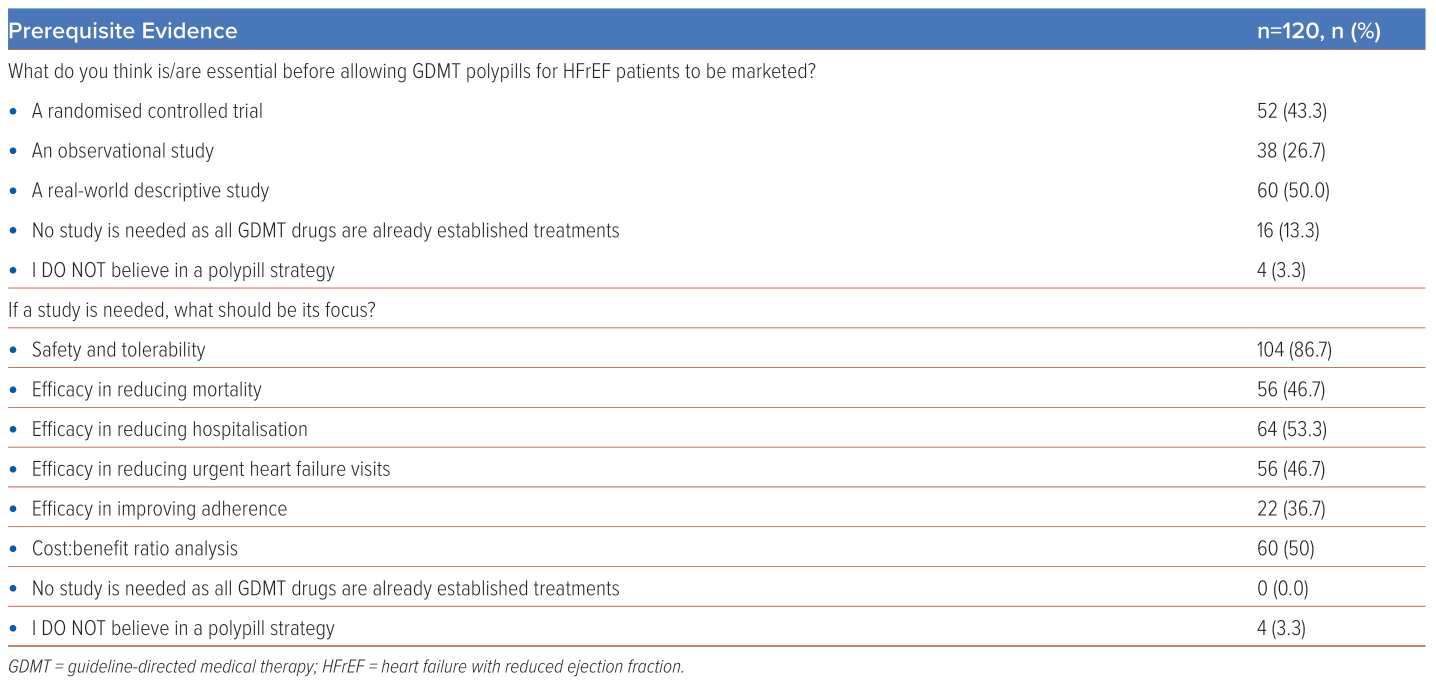
The majority felt that further studies should be undertaken prior to the marketing of GMT-based polypills; either in the form of a real-world descriptive study or randomised control trial (Table 3). Such studies should focus mainly on safety and tolerability (86.7%), efficacy in reducing hospitalisation (53.3%), and on performing cost:benefit ratio analysis (50%). When asked about an ideal combination of heart failure medications, the majority were comfortable with a combination consisting of traditional first-line staples such as BB or RASSI (93.4% stating that it was ‘important’ or ‘very important’ for both classes) or SGLT2I, which have been touted as being both effective and convenient to use.6 There were four respondents (3.3%) who did not believe in a polypill approach, all of whom were male, interventional cardiologists with more than a decade of clinical experience. This minority favoured initiation of GDMT in a stepwise fashion, prioritising BB and RASSI. Major challenges highlighted by this group include potential impact on renal function and cost issues.
This survey demonstrates how implementation of a polypill strategy may remain challenging. Despite updated guidelines stressing the importance of adopting an early, horizontal approach in the initiation of GDMT, a substantial proportion of respondents remain steadfast in their sequential, vertical approach to pharmacotherapy management in heart failure. Although the presence of multimorbidity and associated polypharmacy makes adopting a polypill approach initially appealing, they are also an inherently more complex group of patients with constellation of issues that promote prescription and management inertia.7 Furthermore, with greater appreciation and focus on individualisation of medical care, a one-size-fits-all polypill approach may seem counterintuitive.8 Concerns raised about costs and reimbursement are also important, as currently SGLT2Is are largely purchased out of pocket and are unaffordable for many, which may have an overall impact on the cost–benefit analysis for the development of the polypill, and likely affect the overall pricing strategy for potential polypill combinations as a whole. To tackle clinician inertia, a multi-pronged strategy involving industry, institutions and the health ministry is key in ensuring that clinicians remain educated and updated on the evidence regardless of years of experience, that treatments remain accessible to the masses, and that systems are in place to ensure appropriately timed monitoring can be performed following initiation of treatment, especially in managing heart failure.
There are several limitations to our study. We acknowledge that this survey represents a limited part of our overall cardiology community. Moreover, since it was an open-access survey, selection bias may have occurred. Furthermore, we are unable to ascertain the main areas of practice of responders and individual levels of interest in the field of heart failure, which may influence response. Additionally, responses from non-doctors were not obtained, which could have potentially enriched the quality of our data.
In conclusion, the survey study highlights several important issues raised by cardiologists and cardiology FIT across the nation surrounding GDMT prescription, and the potential issues that may arise following the introduction of a HFrEF polypill. The information gathered will prove useful in determining the prospects of implementing such a strategy regionally. 
Clinical Perspective
- Rapid initiation and uptitration of heart failure medication is currently advocated.
- A polypill strategy is an enticing way to tackle prescription inertia.
- However, its implementation likely remains challenging, especially in Asia.










