For patients undergoing evaluation for suspected acute coronary syndrome, with clinical presentation and troponin profile that is not thought consistent with MI and therefore not undergoing early angiography, current guidelines recommend subsequent functional cardiac testing. The basis for this recommendation, however, arises from an era where biomarkers of myocardial injury had a much lower negative predictive value and is founded on limited clinical data. The perceived evidence for functional testing (e.g. exercise stress testing or exercise or pharmacological stress echocardiography/nuclear scanning) when invasive coronary angiography is not deemed appropriate arose from chest pain assessment units comprising a package of care with protocolised assessment and interventions. Farkouh et al. found, by randomising 424 patients with suspected unstable angina to hospital admission (with individualised management) versus chest pain assessment unit admission in the Emergency Department (ED; with ST monitoring, aspirin, heparin administration and a functional test), that there were no significant differences in primary outcome (non-fatal MI, death, acute congestive heart failure, stroke, out-of-hospital cardiac arrest) within 30 days.1 This suggests that while a comprehensive approach to chest pain assessment may be efficient, low event rates represent little opportunity to further impact outcome. Inherently, this study was not a test of the incremental diagnostic benefit of functional studies. The question of performing a functional study versus no functional study has not been subject to a randomised comparison. Further, there is heterogeneity across Australian, European and US guidelines regarding the recommended approach to subsequent cardiac testing for the diagnosis of coronary artery disease, which places significant burden on the healthcare system in time, resources, iatrogenic risk to the patient and cost.2–4
With the commonplace use of high-sensitivity troponin assays demonstrating a high negative predictive value, the incremental value of routine functional testing in this context is not well defined. With this higher sensitivity, these assays now identify a larger number of patients with detectable troponin concentrations, for whom the clinical presentation is not highly suggestive of a type 1 MI. Given the large group of patients with persistent diagnostic uncertainty, the interaction between routine functional testing, informed by the level of detected troponin, needs further clarification to guide the rational use of limited resources. Therefore, this analysis explores the relationship between receipt of subsequent functional testing and the peak observed troponin level among patients not deemed to be clearly associated with type 1 MI and, therefore, not proceeding directly to invasive coronary angiography.
Methods
Study Design
This was a retrospective analysis of episodes of care for patients who were assessed for chest pain due to suspected MI in Flinders Medical Centre ED (Adelaide, SA, Australia) from 2011 to 2018 using data linkage to evaluate subsequent clinical outcomes. We performed an inverse probability weighted analysis to examine the question of whether functional testing reduces death or MI within 30 days. Ethics approval for access to these data was granted by the Southern Adelaide Clinical Human Research Ethics Committee.
Study Population
Participants who were included were adults aged ≥40 years and ≤80 years, who presented with chest pain or dyspnoea due to suspected ischaemic heart disease, with no prior history of ischaemic heart disease and received at least one troponin test. Focusing on a group of patients with persistent diagnostic and risk uncertainly, we included patients who did not proceed directly to coronary angiography (i.e. high diagnostic suspicion for MI), with peak troponin T of <100 ng/l in the initial assessment period. Further, attempts were made to exclude patients with clinical characteristics known to influence both subsequent invasive or functional testing, including no troponin drawn, prior coronary artery disease, known cancer, prior peripheral vascular disease, prior admission for renal disease, prior cardiac valve surgery and prior revascularisation. Demographic information was recorded, as was past medical history of previous coronary disease, previous cardiac disease (e.g. cardiomyopathy, atrial fibrillation), hypertension, diabetes mellitus, hyperlipidaemia and current smoking status. The troponin peak was recorded.
System-level Troponin T
The Roche Diagnostics Elecsys 5th generation high-sensitivity cardiac troponin T (hs-cTnT) assay (Cobas; Basel, Switzerland; level of detection 5 ng/l, 99th percentile 14 ng/l) was implemented as the sole troponin assay available within all South Australian public hospital EDs. At the time of initial implementation (April 2011) and for the duration of this analysis, a lower clinical reporting limit of the 5th generation assay was aligned to that of the previous assay (i.e. masked with the lower reference limit reported as ‘≤29 ng/l’ rather than to report down to the level of detection [5 ng/l]) due to concerns over the likely increase in invasive cardiac testing if low reference limits were deployed. Access to values down to the level of detection was then systematically studied in a prior randomised trial, with no difference in outcomes observed.5 This analysis used values down to 5 ng/l.
Functional Testing
In the functional testing group, three methods were employed: exercise electrocardiography via the standard Bruce protocol, exercise stress echocardiography and dobutamine stress echocardiography.
Data Collection and Outcome Measures
This study examined the composite outcome of death and MI at 30 days. Death is reported as all-cause mortality, and these outcomes were identified through the South Australian Register of births, deaths and marriages, while MI relied on recurrent admission with an ICD-10AM code of I21.
Statistical Analysis
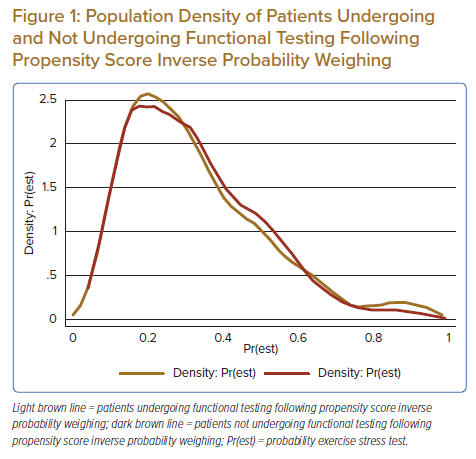
Baseline clinical characteristics are presented as counts and percentages, and compared with c2 testing, while continuous variables are presented as medians and interquartile ranges and compared with Mann–Whitney U-tests. The outcomes of combined death and MI, death, and MI were represented in 2 × 2 contingency tables and compared using the c2 or Fisher’s exact test. To account for clinical selection, we implemented an inverse probability weighted propensity-matched model, with weighting based on a logistic regression model estimating the probability of receiving a functional study based on baseline clinical characteristics (C-statistic 0.72). The patients receiving and not receiving functional testing were weighted based on the inverse of their estimated probability of receiving a functional test. The balance of this weighting was assessed based on the standardised difference between groups, with a difference of <10% considered acceptable. Outcomes by the receipt of functional testing and interaction with peak troponin levels were explored using logistic regression within the weighted cohorts with relative benefits expressed as odds ratios. All statistical analyses were conducted using Stata 15.2, and a p-value of <0.05 was considered statistically significant.
Results
Patient Population and Procedures
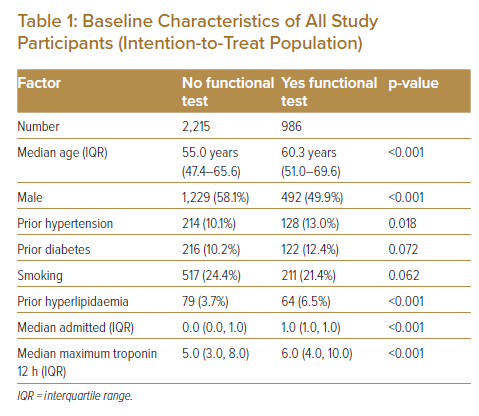
A total of 3,101 patients were included in the final analysis. Of these, 986 underwent functional testing and 2,115 did not undergo functional testing (Table 1). The baseline characteristics show that the median age was 60.3 years in those who underwent functional testing, and 55.0 years in those who did not undergo functional testing. Half the patients (50%) who underwent functional testing were men. The incidence of diagnosis of coronary disease was 2% in both groups.
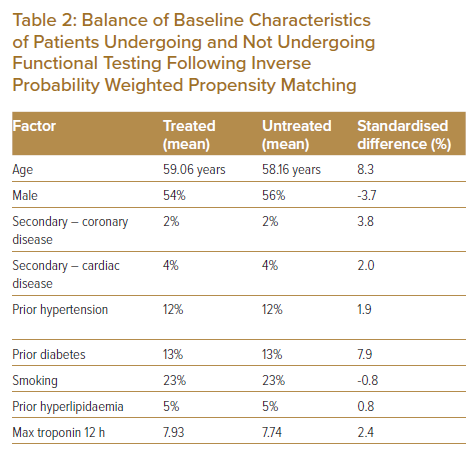
The maximum median troponin at 12 h was 6.0 ng/l in those who underwent functional testing versus 5.0 ng/l in those who did not. The quality of the matching between the two groups was high, as the standardised difference between the groups for each of these covariates was <10%.
Clinical Events at 30 Days
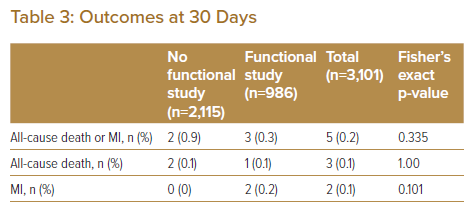
The overall event rate of the primary outcome of all-cause mortality and MI at 30 days occurred in five of the total 3,101 patients (0.16%); two of those who did not undergo functional testing and three of those who did have a functional test. Of 2,115 patients who did not undergo functional testing, there were two events (0.09% of these patients); these were both deaths. Of 986 patients who underwent functional testing, there were three events (0.30%), comprising one death and two acute MIs.
Outcome of Inverse Probability Weighting
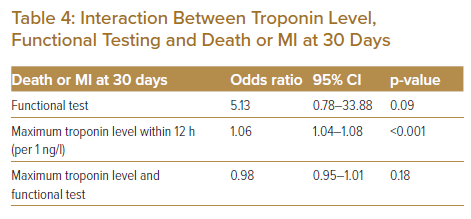
We chose inverse probability weighting for its ability to balance covariates in observational data, where the propensity score is the likelihood that the subject experiences the intervention (Table 2). There was good overlap of those who were predicted to undergo versus those who did not undergo functional testing; Figure 1 shows the propensity density. Within the propensity-matched analysis, there was no difference in the rate of 30-day death or MI between those receiving and not receiving functional testing (Table 3). There was a modest relationship between troponin level and 30-day death or MI; Table 4 shows that for each unit increase in troponin, there was an odds ratio of 1.06 (95% CI [1.04–1.08]; p<0.001) for a higher risk of 30-day death or MI. While there was an increase in the risk of death or recurrent MI with increasing troponin levels, an interaction between the troponin level and an associated reduction in the risk of 30-day death or MI was not observed.
Discussion
In our study, we observed that in an inverse probability-weighted population of 3,101 typical patients presenting with undifferentiated chest pain with persistent diagnostic uncertainty after initial troponin assessment, functional testing was not associated with a reduction in death or MI within 30 days. Importantly, it is in this low-risk group that emergency physicians and cardiologists face the greatest clinical equipoise regarding the diagnosis of IHD and predicting adverse outcomes. The overall event rate of death and MI was exceedingly low (5 patients, 0.16% event rate). Two deaths occurred in those who did not undergo functional testing, and one in whom functional testing was undertaken. Significantly, however, the cause of these deaths was unknown and may not have been due to MI. Functional testing also did not eliminate the risk of acute MI; two of these events occurred, both in patients who did undergo functional testing. Further, the heterogeneity in clinical care and referral to subsequent functional testing highlights the persistent uncertainty regarding the optimal investigative and management strategies among patients with modest troponin elevation. Randomised clinical trials of subsequent diagnostic strategies in this diverse patient group are required.
This low death or MI rate in the low hs-cTnT population is seen in other international studies.6,7 Bandstein et al. studied a retrospective cohort of 14,636 patients who presented to ED with chest pain.6 During 30 days of follow-up in patients with an initial hs-cTnT of 5–14 ng/l (14 ng/l = 99th percentile cut-off), the absolute risk of MI at 30 days was 3.08% (negative predictive value 96.9%; 95% CI [96.3–97.5]); with a death rate of 0.41% (negative predictive value 99.6; 95% [CI 99.4–99.8]).6 Similarly, Neumann et al. found in data leveraged from 15 prospective studies of 23,327 patients across Europe, North America and Australasia, which a very low hs-cTnT at presentation (specifically, 6 ng/l at presentation) and small absolute change on serial sampling (<4 ng/l after 45–120 min) resulted in a high negative predictive value of 99.5% for diagnosis of MI (95% CI [99.2–99.7]), and for MI or death at 30 days (absolute risk 0.2%; 95% [CI 0.2–0.4]).8
Studies have incorporated functional testing for prognosis rather than diagnosis.9 Retrospective and prospective analyses of >420,000 ED encounters for chest pain, in the context of troponin assays pre-dating the current high-sensitivity performance, have shown that patients who did not undergo initial functional testing were no more likely to experience an MI.10,11 The choice of functional test has been variably studied, with those including imaging showing improved testing metrices (discriminative abilities) compared with the exercise stress test.12 Again, these studies highlight the limited opportunity to impact short-term clinical outcomes with the routine use of current testing approaches.
The downstream effects of hs-cTn testing in relation to subsequent testing has been observed in the APACE prospective multicentre diagnostic trial.13 Here, 2,544 patients with suspected MI who presented to EDs in Europe were observed prior to, and after, the introduction of hs-cTn testing in different hospitals. There was a significant incrcease in the diagnosis of MI, a decrease in the diagnosis of unstable angina and decrease in the rate of functional testing.13 Results from this analysis further suggest that the risk stratification provided by hs-cTn, specifically in its ability to exclude unstable coronary artery disease, indicates that a strategy of functional testing among patients with ‘rule-out MI’ troponin profiles may represent low-value care.
Our data were collected in a single centre and, therefore, reflective of practice in this centre. The number of outcome events was small; hence, power was limited. Additionally, pre-test probability was unknown, and risk stratification was not calculated in the analysed population. Outcomes were binary regarding the presence or absence of functional testing and outcomes of death or MI, which did not allow inferences of correlation with positive functional tests or referral for coronary angiography (and downstream effects of that intervention). Further, while attempts were made to restrict the analysis population to those who were likely eligible for functional testing, reasons for not undergoing testing, such as substantial comorbidities, could not be fully excluded. However, any unmeasured comorbidity was not associated with an increase in 30-day events.
Conclusion
Current international guidelines for the investigation of suspected ischaemic chest pain are open to variable interpretability. We found that, in a low-risk population, functional testing was not associated with reduced risk of death or MI within 30 days. These exploratory, propensity-matched data suggest that in those with no known ischaemic heart disease, functional testing within that timeframe may provide limited further diagnostic benefit in the context of high-sensitivity cardiac troponin testing.
Clinical Perspective
- Functional testing for the assessment of acute chest pain has not been re-examined in the era of high-sensitivity cardiac troponin testing.
- Our analysis of patients who underwent assessment for chest pain showed no significant difference in 30-day death or MI between those who underwent functional testing versus those who did not undergo functional testing.
- The ideal strategies for diagnosis, prognosis, and management of patients with chest pain and of high-sensitivity cardiac troponin profile not considered to be due to MI and, therefore, referred for coronary angiography requires reconsideration and research.
- There is opportunity to redesign the historical chest pain assessment pathways with consideration for a shift to peri-hospital outpatient care, including formalised access to downstream testing and a longitudinal cardiovascular risk assessment.