The spontaneous recanalised coronary thrombus (SRCT) is defined as a coronary lesion with multiple intraluminal channels. The appearance of the lesions in imaging findings has been variously described as spider-web like, or resembling Swiss cheese, honeycomb or lotus root. The complexity and structural variability of SRCTs poses challenges in coronary interventions. To date, no uniformity regarding the optimal intervention strategy in SRCT has been described.
We present two cases of optical coherence tomography (OCT)-guided percutaneous coronary intervention (PCI) in SRCT lesions. We emphasise the role of OCT in SRCT lesion recognition, providing insights into optimal lesion preparation and stent implantation. The cases also illustrate the procedural challenges in managing SRCT lesions.
Case 1
A 43-year-old man presenting with shortness of breath on moderate exertion was referred to our hospital for a coronary procedure. He had a history of an MI 3 months earlier, was a smoker and had diabetes. He was treated with furosemide 40 mg, dual antiplatelet therapy (acetylsalicylic acid 80 mg and clopidogrel 75 mg), atorvastatin 40 mg, bisoprolol 2.5 mg, captopril three × 12.5 mg and rapid insulin three × 4 units.
His vital signs were stable. A remarkable physical finding was cardiomegaly without any signs of congestion. ECG showed sinus rhythm with left axis deviation. Transthoracic echocardiography revealed left ventricle (LV) dilatation and marked reduction of LV systolic function with ejection fraction 24%. Dobutamine stress echocardiography showed viable myocardium in all left ventricular segments.
Therapeutic Intervention
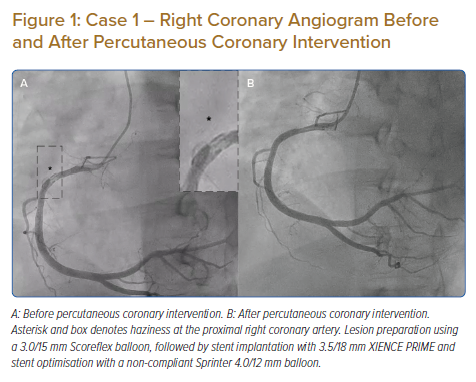
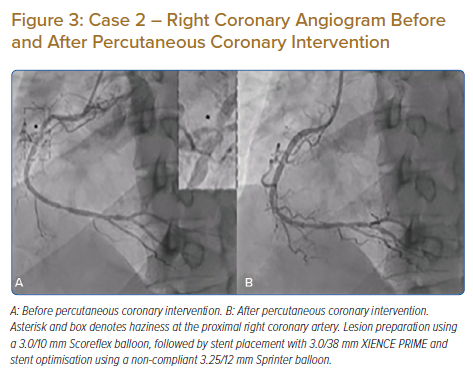
Coronary angiography revealed mild stenosis at the distal left main. Left anterior descending (LAD) evaluation showed moderate-severe stenosis at the mid–distal segment. The left circumflex was normal. Right coronary artery (RCA) evaluation revealed haziness at the proximal part with thrombolysis in myocardial infarction (TIMI) flow grade 3 (Figure 1A). We performed an OCT (Ilumien Optis System) evaluation of the RCA, which revealed channels of recanalised thrombus, divided by fibrous septa with variable thickness and high intensity and low signal attenuation at the proximal RCA (Figure 2A). Lesion preparation was performed using a 3.0/15mm Scoreflex balloon (OrbusNeich). OCT evaluation after scoring balloon dilatation showed adequate plaque disruption. A 3.5/18 mm XIENCE PRIME stent (Abbott Vascular) was implanted. Post-PCI OCT evaluation demonstrated mild stent malapposition (0.5 mm) at the middle part of the stent. Stent optimisation was performed using a 4.0/12 mm non-compliant (NC) Sprinter balloon (Medtronic). Final OCT evaluation showed good stent expansion (minimal stent area 11 mm2) and stent apposition with no stent edge dissection (Figure 2B). Contrast injection showed TIMI flow grade 3 (Figure 1B).
Follow-up and Outcomes
No symptoms or clinical complications were observed after the procedures. The patient was discharged from hospital the following day.
Case 2
A 46-year-old man presented with chronic coronary syndrome. He had a history of PCI of the LAD 1 year before. He smoked and had hypertension. The patient was receiving dual antiplatelet therapy (acetylsalicylic acid 80 mg and clopidogrel 75 mg), atorvastatin 40 mg, bisoprolol 10 mg and ramipril 10 mg.
His vital signs were stable, with no remarkable physical findings. ECG showed sinus rhythm with pathological Q waves in the inferior lead. An echocardiogram revealed mild LV dilatation and reduced LV systolic function (ejection fraction 44%), with hypokinesia on the basal-mid inferior, inferolateral and inferoseptal wall.
Therapeutic Intervention
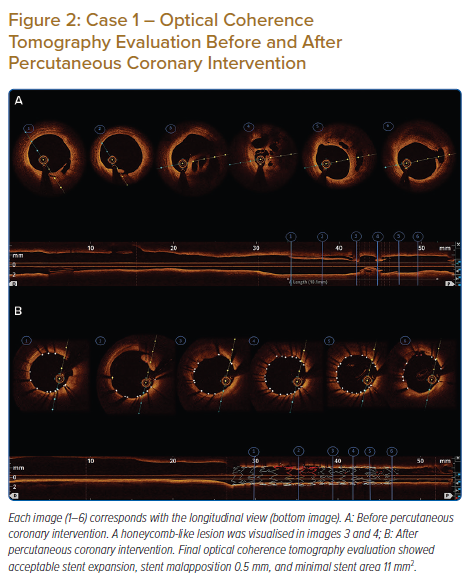
Coronary angiography showed the left main was normal, with a right dominance system. The LAD stent was patent. A chronic total occlusion (CTO) lesion was visualised at the proximal part of the left circumflex. The RCA revealed moderate–severe stenosis at the mid part of the RCA with haziness (Figure 3A). We decided to perform fractional flow reserve (FFR) evaluation on the RCA before intervention.
The FFR wire was introduced to the RCA, but it failed to cross the lesion. We exchanged the wire for a Runthrough NS Floppy wire (Terumo). After several unsuccessful attempts crossing the lesion, we finally successfully crossed the lesion with the support of a Corsair 135 (Asahi) microcatheter. Considering prior wire crossing difficulties despite the angiography only showing moderate–severe lesions, we decided to perform intracoronary evaluation by OCT.
Pre-PCI OCT evaluation revealed a lesion with multiple channels of organised thrombus, divided by fibrous septa with variable thickness and high intensity/low signal attenuation, mimicking honeycomb features (Figure 4A). In light of this, we decided to intervene in the RCA.
Lesion preparation was performed using a 3.0/10 mm Scoreflex balloon to disrupt the fibrous septa. Post-scoring-balloon dilation OCT evaluation showed adequate plaque disruption. Therefore, it was followed by stent placement with a 3.0/38 mm XIENCE PRIME. Post-stenting OCT evaluation revealed stent malapposition at the proximal part, so we performed stent optimisation using a 3.25/12 mm NC Sprinter balloon. Final OCT evaluation showed good stent expansion and apposition (minimal stent area 6.9 mm2) and no stent edge dissection (Figure 4B). Contrast injection showed TIMI flow grade 3. FFR calculation was 0.89, without any complications (Figure 3B).
Follow-up and Outcomes
No symptoms or clinical complications were observed after the procedures. The patient was discharged from hospital the following day.
Discussion
SRCT is characterised by lumen irregularities with a braid-like appearance detected by intracoronary imaging. It was first observed by Terashima et al. in 2002 in patients with Kawasaki disease.1,2 The incidence and prevalence of SRCT are unknown. The pathological mechanisms are still unknown, but possibilities include spontaneous recanalisation of the thrombus because of plaque erosion, plaque rupture, coronary dissection or coronary thromboembolism.2,3 Suzuki et al. described the histopathologic assessment of septa as bilateral endothelial layers with collagen and elastin fibres between them.4
Intracoronary imaging allows detailed coronary lesion characterisation, guiding the PCI strategy and optimisation. OCT uses the scattering and absorption of near-infrared light, providing adequate tissue penetration with excellent axial and spatial resolution resulting in detailed identification of plaque characteristics and composition in real time. Intracoronary imaging of SRCT shows signal-rich, high-backscattering diaphragm-like protrusions, dividing the lumen into multiple small channels separated by fibrous septa, representing remnants of a late-stage recanalised thrombus.4 The fibrous septa were composed of high signal intensity and low signal attenuation, suggesting elastin and collagen fibres, as in our cases.4
The complexity and potential structural variability of SRCT pose challenges for coronary interventions. We encountered difficulties advancing the wire to cross the lesion in our second case. There are several possible causes of wiring difficulty in non-CTO lesions, such as severe tortuosity, extensive calcification, and severe stenosis or subtotal occlusion.5 However, in our cases, OCT revealed multiple channels of recanalised thrombus. Thus, the wiring difficulties may be caused by the complex architecture of the lesion, making the tangled yet narrow intraluminal channels.

Typically, step-wise approaches for difficulty wiring non-CTO lesions begin with first-line wire choices: a spring-coiled, hydrophobic, low gram workhorse wire. Escalating to an alternative wire is necessary after attempting and failing with a workhorse wire. However, the wire selection differs with specific conditions. Furthermore, using a wire support should also be considered.5
We suggest performing the sliding entry technique to facilitate tracking the channel of the SRCT lesion, as in our case. Regular floppy wire or hydrophilic wire is advanced with gentle tip rotation and probing to slide through the channel of recanalised thrombus, as opposed to tracking a microchannel in CTO lesion, which usually uses tapered wires. We also recommend considering using a microcatheter or balloon to increase wire support while crossing the lesion and to reduce the likelihood of wire tip deflection.
Unfavourable PCI outcomes have been described in SRCT lesions, such as in-stent thrombosis and in-stent restenosis.6 The primary factors contributing to stent failures are inadequate stent deployment and incomplete stent apposition, resulting from inadequate lesion preparation.7 Therefore, our strategy was to perform optimal lesion preparation in our cases.
There are several lesion preparation strategies for dealing with coronary lesions, such as using balloon dilatation (NC balloon, ultrahigh-pressure balloon, modified balloon), atherectomy devices or intravascular lithotripsy, the choice of which depends on specific scenarios. The NC balloon allows transmission of high pressures to resistant lesions while maintaining its shape and volume; therefore, the force is directed to the lesion rather than transmitting it to other artery parts, as with semi-compliant balloons. The cutting balloon is an NC balloon with atherotomes along the surface that can cut into the plaque, creating controlled dissection and crack propagation. The scoring balloons consist of balloon-mounted spiral scoring wires that anchor into fibrocalcific plaque.8,9
Despite these advances, to date there are no evidence-based data regarding the effectiveness of lesion preparation across various balloon dilation methods. We opted for the Scoreflex balloon as the method of lesion preparation because of the complex anatomy of SRCTs, particularly the presence of relatively thick fibrous septa. Compared with the NC balloon, whose force tends to be distributed to the segments with less resistance, Scoreflex, with its built-in integral wire and the coronary guidewire on the outside of the balloon, creates a focused force in a localised region of the plaque. The Scoreflex balloon can facilitate controlled plaque disruption.9 The Scoreflex balloon sizes were calculated using reference diameter from the OCT.
Adequate lesion preparation was shown by post-scoring balloon dilation OCT evaluation, characterised by complete disruption of the fibrous septa. In both cases, OCT-guided optimal stent implantations were successfully achieved after adequate lesion preparation.
Conclusion
The recanalised coronary thrombus can potentially become an obstacle in coronary interventions because of the complexity of the anatomy. To optimise PCI results, lesion preparation should be considered in managing recanalised coronary thrombus lesions. OCT may guide treatment decisions before, during and after PCI, giving optimal results.
Clinical Perspective
- Intracoronary imaging has provided insight into coronary lesions and vessel morphology, which plays a pivotal role in the optimisation of percutaneous coronary intervention.
- Recanalised coronary thrombus should be considered as a cause of hazy intracoronary angiographic images.
- Several procedural challenges may be encountered during percutaneous coronary intervention on spontaneous recanalised coronary thrombus lesions, such as wiring difficulties and opting for appropriate methods of lesion preparation, so physicians should have knowledge in dealing with lesions of this type.