Background
Severely calcified lesions are associated with increased procedural risks and suboptimal results such as stent underexpansion.1 Stent underexpansion is often related to stent thrombosis and in-stent restenosis (ISR).2 Conventional treatment of native non-dilatable calcified lesions is well established with rotational atherectomy (RA), and more recently with shockwave intravascular lithotripsy (IVL). Stent ablation by RA for the management of non-dilatable stent underexpansion is an off-label strategy and has been reported in limited case series.3
The principle of stent ablation by RA of underexpanded stent relies on modification of both stent and underlying calcium, through the differential cutting mechanism. Thus, fragmentation and debulking of the calcified plaque underneath the stent struts allow the artery to become compliant for further modification by balloon dilation strategies. This principle can be applied not only for non-dilatable underexpanded stents but also for resistant, balloon-uncrossable lesions across the stent struts in a calcified bifurcation lesion. This facilitates easy delivery of devices across the struts into the side branch (SB) and adequate lumen restoration of the main vessel (MV) and SB.
Stent ablation procedure by RA has previously been described in the literature with limited case reports and series.3 However, there are no previous case studies of stent ablation procedures across the stent struts. The present case series describes the use of RA for non-dilatable lesions within underexpanded stents and across the stent struts (across stented bifurcation) and the technical differences between the two.
Methodology
Study Population
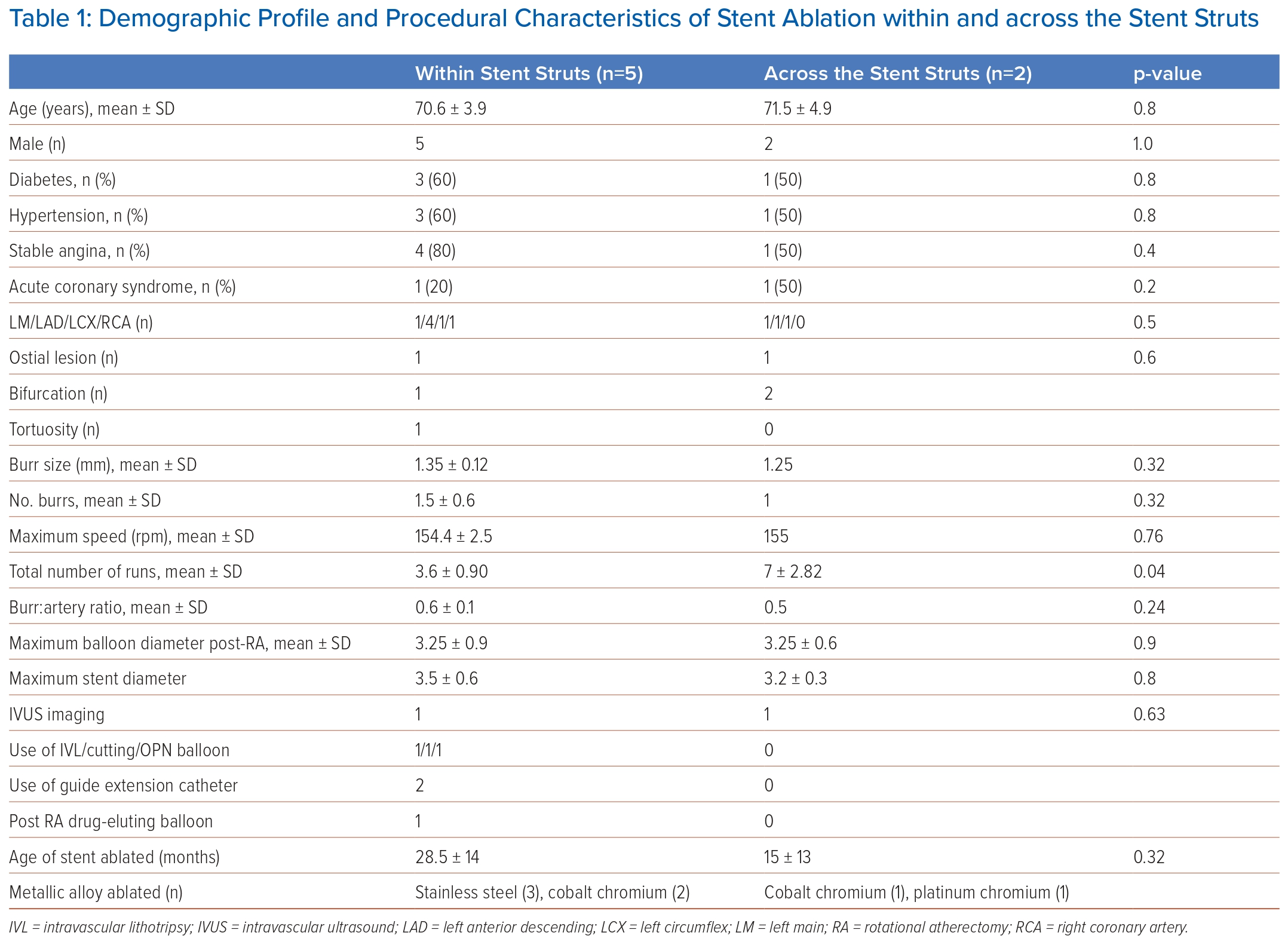
The study retrospectively analysed a total of 790 patients who had undergone RA procedure at a single tertiary care specialist cardiovascular centre between 2015 and 2022. Of these patients, seven had stent ablation procedure.
Data were collected as part of the institution’s audit and quality improvement program and were anonymised for analysis. Use of anonymised data for research was exempted from review by the institutional ethics board.
The indication for revascularisation was either acute coronary syndrome (ACS) or chronic stable angina (CSA). Two groups are described: RA within underexpanded stents (group 1) and across the stent struts (across stented bifurcation; group 2).
Intervention Procedure
The procedures were performed by experienced operators in RA either through a radial or femoral approach. Stent ablation was performed when there is persistent ‘dog-bone’ effect of non-compliant (NC) balloon due to stent expansion failure or resistant lesion across the stented bifurcation lesion.
The RotaLink Plus system (Boston Scientific) was used to perform RA and standard 0.009" extra support rota wire was used in all the cases. The rotational speed was set between 150,000 and 160,000 rpm and time of ablation run was limited to 15 seconds per run.
Statistical Analysis
Continuous variables were represented by mean ± SD and in numbers for categorical data. Pearson’s χ2 test was used for categorical data and Student’s unpaired t-test was applied to quantitative variables; p <0.05 was considered significant. SPSS 21.0 was used for data analysis.
Results
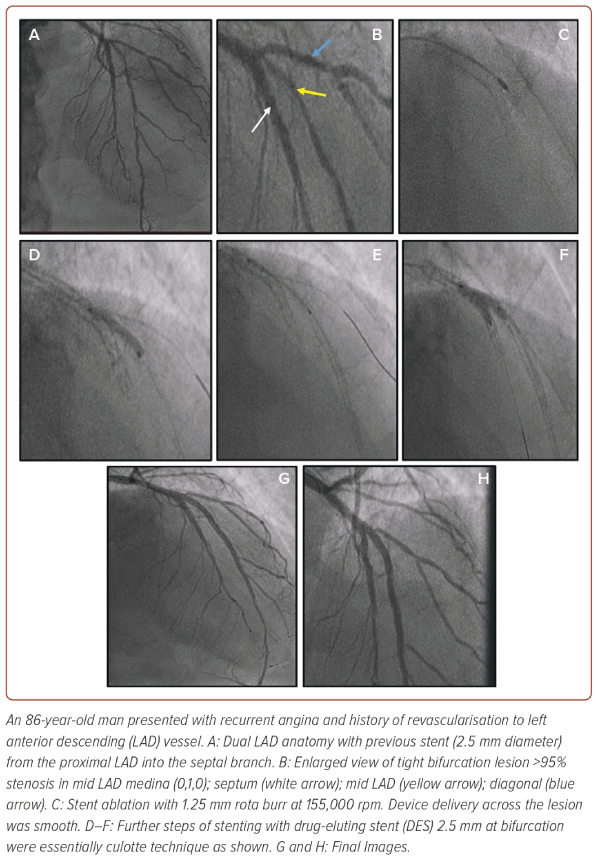
The procedural characteristics are shown in Table 1. The initial size of the burr used was 1.25 mm in all cases except one, where a 1.5-mm burr (burr:artery ratio 0.5) was used for stent ablation across the left main (LM) into the circumflex (LCX) artery. Upsizing of burr was done in two cases in group 1 (Figure 1).
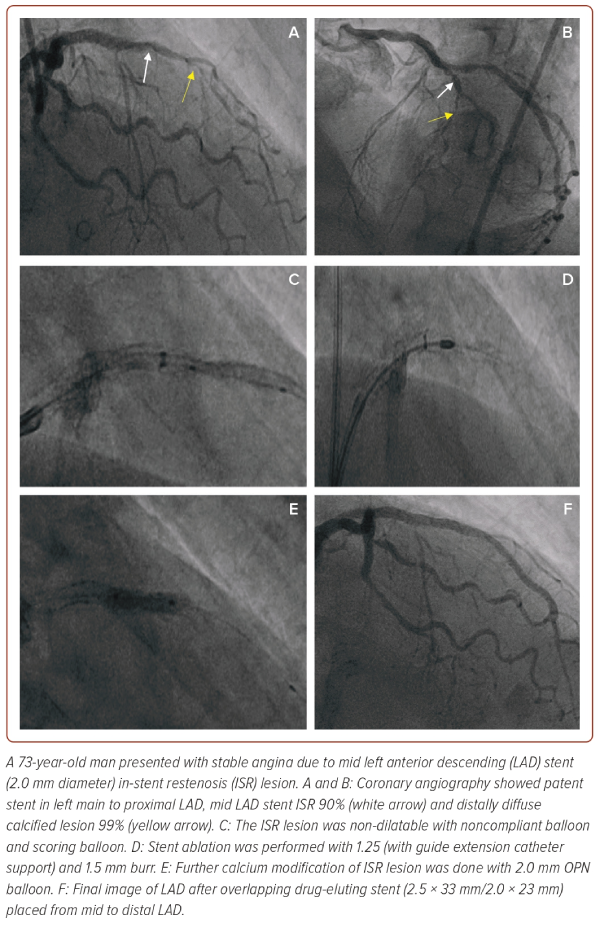
The burr:artery ratio was 0.6 ± 0.1 in group 1 and 0.5 in group 2 (p=0.24). The maximum rotational speed was 154,400 ± 2,500 and 155,000 rpm in the two groups. The total number of RA runs was 3.6 ± 0.90 in group 1 and 7.0 ± 2.8 in group 2, respectively with p=0.04. A d7 Fr guide extension catheter was used in two cases to prevent burr exposure to proximal vessel tortuosity and proximal vessel non-target stent struts.
The procedural endpoint was achievement of full expansion of NC balloon (sized to the normal diameter of reference stent) following stent ablation. Drug-coated balloon (DCB) or drug-eluting stent (DES) was used depending upon the vessel size and location of target lesion. Procedural success was achieved in all cases with no complications. There were no occurrences of slow-flow, no-reflow or burr entrapment.
Clinical follow-up was at 30 days and 1 year. At 30 days there were no events, including death, MI or target lesion revascularisation (TLR). At 1 year, one of seven patients (14%) had TLR. There were no deaths. We observed one death of noncardiac origin in the third year of follow up.
Discussion
Treating stent underexpansion with an underlying mechanical cause of heavy calcification is complex and may be associated with complications such as perforation, vessel rupture or technical failure. Stent underexpansion resistant to high-pressure inflations by NC balloon has limited therapeutic options like ultra-high pressure balloon inflation with OPN balloon, IVL, RA and excimer laser coronary angioplasty (ELCA). The use of OPN balloons does carry some risk of vessel rupture or perforation at the vessel wall opposite areas of severe calcification. The use of IVL can address areas of concentric calcification but may be less useful in areas of nodular calcification although anecdotally may have some effects. However, in some cases, the IVL catheter may not easily reach the target lesion if it is too distal, due to the bulkier nature of the balloon.
The procedural characteristics of stent ablation were similar between the two groups, except that the total number of runs required was higher with stent ablation across group 2. This is suggestive of relatively more time taken for the burr advancement across the full thickness of the stent struts. The relative angle between the SB and MV and the stent struts in the path of RA would act as restraining mechanical factors slowing the burr speed and risking burr entrapment. Thus, the operator had to be extra cautious and patient to avoid excessive decelerations of the burr and the ‘watermelon seed’ phenomenon. Excessive pushing of the burr should be avoided.
The first case of stent ablation across the stent struts (Figure 2) is a typical example of a balloon uncrossable lesion at bifurcation lesion with stent struts across (group 2). The possible reason for the difficult delivery of device across the mid left anterior descending (LAD) was the presence of calcium and metallic stent struts in the way of ablation. Thus, stent ablation enabled the modification of uncrossable bifurcation lesion and made the further steps of the procedure easier.
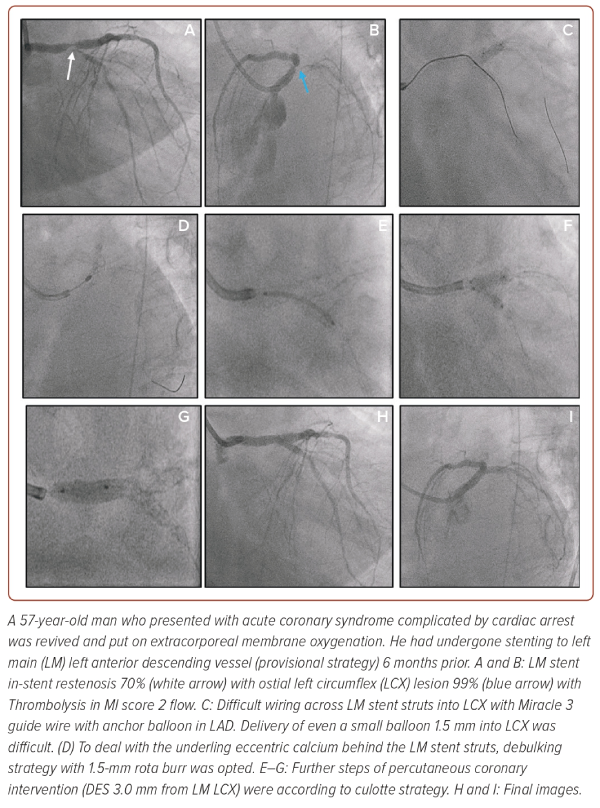
The second case (Figure 3) is another example of treatment of the left main ISR lesion with underlying calcium being the culprit for stent underexpansion leading to subtotal occlusion of the left circumflex ostium. Device delivery into SB across the stent struts was difficult due to the stent struts and underlying calcification. In this case, delivery of IVL across the stent struts would have been difficult task. To manage this, the calcium modification underneath the stent struts with RA was performed. Thus, with the stent ablation strategy, adequate lumen gain and reconstruction of calcified bifurcation ISR lesion was achieved.
The most feared complication of stent ablation is burr entrapment with a reported incidence of around 0.00–9.1%.4 This risk would be higher in cases with stent struts in the way of ablation and possibility of ‘watermelon seed’ phenomenon. The occurrence of burr entrapment can be minimised with considerations like starting the ablation with a smaller burr, slow forward motion to sandpaper the stent, shorter runs to reduce heat production, keeping the rotational speed in the range of 150–160 rpm and application of minimum required forward pressure to avoid decelerations. In our case series, the burr:artery ratio was between 0.5 and 0.6 and the maximum speed of burr was in the range of 150–160 rpm to minimise the complications.
Limitations
The main limitations of the study were its small sample size and retrospective nature. Furthermore, the cases described involved stents implanted at different time periods from the RA procedure. Stent types included stainless steel and cobalt chromium. The effect of metallic debris from different metals, polymer and drugs in distal vasculature could not be assessed in this study.
Conclusion
RA is a promising bailout option for resistant non-dilatable lesions within and across the stent struts. When performed carefully, it is a safe and effective strategy to manage this difficult anatomic subset. 
Clinical Perspective
- This case series describes the technical aspects of performing stent ablation procedure by rotational atherectomy (RA) and compares the use of RA for non-dilatable lesions in two anatomical categories.
- Stent ablation across the stent struts is technically more challenging in comparison with ablation within the stent.
- RA procedure could be safely and successfully performed in experienced hands by considering some precautions to prevent burr entrapment.